Figure 1. Tense hemorrhagic bullae developed over the course of the patient’s disease. Tender purpuric papules on the palms and marked hand swelling are also apparent.
Eosinophilic granulomatosis with polyangiitis (EGPA) is an anti-neutrophil cytoplasmic antibody-associated vasculitis typically characterized by asthma, peripheral eosinophilia and medium- to small-vessel necrotizing vasculitis. Cutaneous manifestations in EGPA are diverse. Palpable purpura is the most common presentation, but urticaria, erythematous macules and papules, livedo reticularis, digital necrosis and cutaneous nodules have also been described.1 Non-hemorrhagic bullae are a rare initial manifestation of EGPA.2-5
Case Presentation
A 58-year-old woman with a history of adult-onset asthma and sinusitis presented with an acute bullous skin eruption. She had been prescribed amoxicillin-clavulanate for ear pain; however, after five days of antibiotic therapy, she developed pruritus overlying her chest and neck. Over the next few days, she developed diffuse extensive painful bullae and erythematous plaques.
On initial presentation to the emergency department, she did not have other symptoms and appeared systemically well. Dermatologic examination was significant for diffuse erythematous, edematous, well-circumscribed papules and plaques, with overlying vesicles and tense bullae. She had no mucous membrane involvement. Laboratory tests were unremarkable except for an elevated eosinophil count of 2.3×109 cells/L (reference range [RR]: <0.8×109 cells/L) and C-reactive protein (CRP) of 45 mg/L (RR: <3.1 mg/L). Her renal and liver functions were normal.
Provisional diagnoses included immunobullous disease, such as drug-induced bullous pemphigoid or linear IgA bullous dermatosis. A drug rash, with eosinophilia and systemic symptoms, and Stevens-Johnson syndrome were considered unlikely given the lack of systemic symptoms and mucous membrane involvement.
Lesional and perilesional skin biopsies were obtained. The patient was instructed to discontinue amoxicillin-clavulanate. She was discharged home on clobetasol propionate 0.05% ointment, with close outpatient follow-up.
Four days later, she returned with new-onset, tense hemorrhagic bullae on bases of painful, purpuric and palpable plaques (see Figures 1, above, & 2, opposite). Tender, violaceous and edematous plaques were present on her palms and soles. She also described pedal edema and chest pain. She had no constitutional symptoms. She was tachycardic at a rate of 120 beats per minute, with a low blood pressure of 98/64 mmHg.
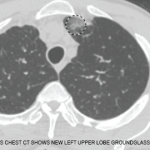
In addition to her skin eruption, the examination was significant for splinter hemorrhages and nailfold capillary hemorrhages. Investigations revealed an eosinophil count of 4.2×109 cells/L (RR: <0.8×109 cells/L), CRP of 87 mg/L, troponin-T of 542 ng/L (RR: <9 ng/L) and N-terminal pro-brain natriuretic peptide of 1,438 ng/L (RR: <300 ng/L). No liver or renal impairment was seen. Her electrocardiogram showed sinus tachycardia. Given her history of adult-onset asthma, sinusitis, ear pain, nailfold hemorrhages, new purpura, hemorrhagic bullae and myocarditis, she was clinically diagnosed with EGPA. She was treated with 1 g of intravenous methylprednisolone daily for three days.
Skin biopsy later confirmed leukocytoclastic vasculitis with extensive eosinophilic infiltration and bulla formation. Direct immunofluorescence was negative at the dermal-epidermal junction. The presence of perivascular accumulation of IgG, IgA, IgM, C3 and fibrin was consistent with vasculitis. The distribution of immunofluorescence was not in keeping with systemic lupus erythematosus. No flame figures were seen. These findings were consistent with EGPA. Her myeloperoxidase titer was elevated at 75 IU/mL (RR: <3.5 IU/mL).
EGPA is typically not considered in the differential diagnosis of patients presenting with non-hemorrhagic bullae unless other clinical features are present.
Other investigations revealed an elevated rheumatoid factor of 288 IU/mL (RR: 0–20 IU/mL), normal C3 and C4 and negative cryoglobulins. Her renal function remained normal, with no proteinuria or cellular sediment. She was incidentally found to be hepatitis B positive with a viral load of 112 IU/mL and was started on tenofovir.
Following intravenous methylprednisolone, she was transitioned to 60 mg of prednisone daily with an outpatient taper. Intravenous cyclophosphamide was started and continued per the European Vasculitis Society protocol.6 With treatment, her skin lesions improved. Her troponin, eosinophilia and CRP also improved, and she was discharged home.