Here, we present a case of a previously healthy woman admitted with acute dyspnea on exertion, which raised suspicion for COVID-19 despite her first test being negative.
Because no specific or pathognomonic imaging findings exist to differentiate GPA from other conditions, suspicion for the disease should arise from clinical presentation and serologic markers.
Cryptogenic Organizing Pneumonia
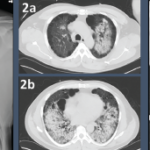
COP, previously called bronchiolitis obliterans organizing pneumonia, is an interstitial disease that affects the distal airways, primarily bronchioles and alveoli. Disease onset occurs between the fifth and sixth decades of life, and it affects men and women equally. Patients present with non-specific symptoms of relatively short duration (weeks to months), such as fever, cough and dyspnea. There are three described imaging patterns of COP, but the typical pattern consists of patchy alveolar opacities ranging from groundglass opacities to consolidation with air bronchograms. These are usually bilateral and peripheral and may wax and wane just like in GPA. In contrast to other interstitial lung diseases, COP does not have honeycombing.6
Diagnosis of COP can be challenging since as the name suggests, the physician must ensure it is cryptogenic in origin and not secondary to an underlying disease. A long list of diseases and medications is associated with the typical histopathological features and imaging findings of COP. Therefore, a careful evaluation of the patient’s underlying diseases, environmental exposures, medication use, physical examination and ancillary tests is required to determine if the organizing pneumonia is cryptogenic in nature. Differentiating between lung-limited GPA and COP can be challenging, because both conditions are radiographically indistinguishable. Organizing pneumonia has also been described as a rare variant of GPA, which has similar clinical, radiographic and even histologic findings. It can sometimes be distinguished from GPA by the absence of extensive areas of geographic necrotizing granulomatous inflammation.7
Summary
Any patient presenting with respiratory symptoms in the current climate raises suspicion for COVID-19, but other etiologies should always be considered. Although our patient’s acute onset of respiratory symptoms with the presence of groundglass opacities and consolidations on imaging were concerning for COVID-19, a thorough evaluation of other potential etiologies, including GPA, cryptogenic organizing pneumonia, other idiopathic interstitial pneumonias, hypersensitivity pneumonitis and DAH, was performed to arrive at her diagnosis. Ultimately, the combination of multiple COVID-19 tests to rule out a false negative, the lack of response to antibiotics, positive serologies, a good response to steroids and CT findings helped rule out infection and establish the diagnosis of GPA.