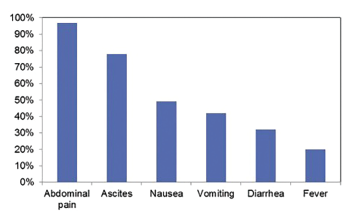
Figure 3: Incidence of Symptoms at Presentation with Lupus Enteritis3
Since 2015 she has had intermittent flares, attributed to SLE, with rashes on her hands and joint pain, predominantly in her hands. Flares tended to be cyclic and related to her menses. She self-managed her symptoms with stress reduction and homeopathic modalities. She had no recent hospitalizations or steroid tapers. She did not think her current symptoms were typical of an SLE flare, and she was taking no medications at the time of presentation.
Review of Systems
The patient had chronic hair loss, difficulty taking a deep breath due to abdominal pain, esophageal reflux, abdominal pain, nausea, vomiting, diarrhea, anorexia, rash on her hands and an oral ulcer. She denied fevers, chills, weight loss, joint pain or swelling, chest pain, headaches, vision changes, dyspnea, dysuria, hematuria, weakness, leg swelling, seizures, blood clots, miscarriages, recent travel, sick contacts, a history of inflammatory bowel disease or Raynaud’s phenomenon.
At presentation, she was not sexually active and denied sexually transmitted illnesses in the past and no recent exposures. She denied tobacco, alcohol and drug use.
Physical exam: On examination, the patient’s blood pressure was 114/88. Her heart rate was 100 beats per minute, and her respiratory rate was 20 breaths per minute, with an SpO2 of 99% on room air. Her temperature was 36.5ºC (97.7ºF). She weighed 59.6 kg (131 lbs.) and had a BMI of 24.04 kg/m².
General: The patient was alert, awake and oriented to person, place and time. She could carry out normal conversation. She appeared uncomfortable lying in bed. The examination of her head, eyes, ears, nose and throat (HEENT) revealed moist mucous membranes and oral ulceration in the posterior pharynx on her left side. Her neck was supple, without lymphadenopathy, and she demonstrated adequate range of motion. Her lungs were both clear to auscultation. She had no wheezes or crackles. She had a regular heart rate and rhythm, and normal S1 and S2 heart sounds, with no murmurs, rubs or gallops.
She had hypoactive bowel sounds. Her abdomen was soft, distended and diffusely tender, including rebound tenderness. She had no organomegaly.
Her extremities were well perfused, with no edema. Her sensation was grossly intact. No tenderness or swelling was appreciated in any joints of her hands, wrists, elbows, shoulders, hips, knees, ankles or feet.
She had mild hair thinning, no scarring alopecia and no malar rash. Her hands were cool to touch, and she had small, blanching macules on her palmar surface and the sides of her fingers. She had no other rashes.
Blood tests: CBC: Her white blood cell count (WBC) was 10,500 cells/µl, her hemoglobin was 13.9 g/dL, her platelets were 255,000 cells/µl, her absolute neutrophil count was 9,100 cells/µl, and the absolute lymphocyte count was 500 cells/µl. Her liver function tests, creatinine kinase and a lipase were normal. Her albumin was low, at 2.5 g/dL (normal range, 3.9–5.5 g/dL). Her creatinine was 0.97 mg/dL and rose to 1.38 mg/dL on a subsequent check. The erythrocyte sedimentation rate was 15 mm/hr, and her C-reactive protein was 2.7 mg/dL (upper limit of normal 0.8 mg/dL). A urinalysis showed a specific gravity of 1.06, small blood and 30 mg/dL protein. Urine microscopy showed 2–5 red blood cells. Clostridium difficile testing was negative. Her thyroid-stimulating hormone (TSH) level was 16.2 uIU/mL with a normal free T4 (1.34 uIU/mL). Blood cultures and tests for enteric pathogens were sent.
Imaging: An abdominal ultrasound taken during the patient’s emergency department visit three days earlier showed mild prominence of the right renal collecting system, without visualized obstruction. No other acute sonographic findings of the abdomen were revealed.
Computed tomography (CT) of the abdomen and pelvis revealed diffuse gastroenteritis, with wall thickening involving the stomach, duodenum, small bowel and colon (see Figure 1). Mucosal hyperenhancement demonstrated a target-like appearance. Mildly complex ascites and extensive mesenteric fat stranding were apparent. Mild wall thickening of the peritoneum raised the possibility of concomitant peritonitis. The CT showed patent abdominal vasculature, no pneumoperitoneum, pneumobilia or portal venous gas. There was mild, bilateral hydroureteronephrosis, with subtle enhancement of the ureteral urothelium. An X-ray of the chest (see Fig. 2) revealed new, small, bilateral pleural effusions and low lung volumes with mild bibasilar atelectasis.

