| SLE Related | Non-SLE Related |
|---|---|
| Lupus enteritis | Appendicitis |
| Pancreatitis | Lithiasic cholecystitis |
| Pseudo-obstruction | Peptic ulcer |
| Acalculous cholecystitis | Acute pancreatitis |
| Mesenteric thrombosis | Retroperitoneal hematoma |
| Hepatic thrombosis | Ovarian pathology |
| Medications (NSAIDs, MMF, steroids, HCQ …) | Diverticulitis |
| Colon perforation (vasculitis) | Adhesions, intestinal occlusion |
| Infectious enteritis | |
| Pyelonephritis | |
| CMV colitis |
Key: NSAIDs: non-steroidal anti-inflammatory drugs; MMF: mycophenolate mofetil; HCQ: hydroxychloroquine.
Table 2: Anatomic Distribution of GI Involvement among Patients with SLE2
| Organ | Involvement |
|---|---|
| Mouth/pharynx | Oral ulcers |
| Esophagus | Dysphagia Esophageal dysmotility Gastric reflux Bullous epidermolysis Ulcerative esophagitis |
| Stomach | Peptic ulcer disease Gastric enteritis Dyspepsia |
| Pancreas | Acute pancreatitis |
| Liver | Hepatomegaly Type 1 autoimmune hepatitis Steatosis Nodular regenerative hyperplasia |
| Gallbladder | Primary sclerosing cholangitis Autoimmune cholangiopathy Acute acalculous cholangitis |
| Small Intestine | Celiac disease Mesenteric vasculitis Protein-losing enteropathy Cytomegalovirus enteritis Intestinal pseudo-obstruction |
| Colon | Crohn’s disease Bowel perforation Pneumatosis cystoides intestinalis Benign pneumoperitoneum |
| Rectum, anus | Ulcerations |
| Other | Appendicitis Primary lupus peritonitis Splenomegaly Ascites |
Lupus Enteritis
According to the BILAG 2004 definition, lupus enteritis is either vasculitis or inflammation of the small bowel with supportive imaging and/or biopsy findings.4 It may also be called mesenteric arteritis, intestinal vasculitis, enteric vasculitis, mesenteric vasculitis, lupus peritonitis or abdominal serositis.
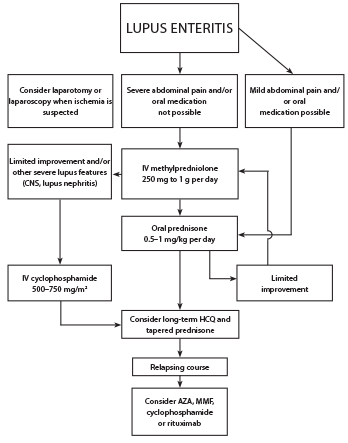
Figure 4: Proposed Treatment Algorithm for SLE Patients with Lupus Enteritis3
Although the pathogenesis of lupus enteritis remains unknown, it has been reported that immune complex-mediated visceral vasculitis may result in bowel wall and mucosal edema.5 The most common clinical manifestations include abdominal pain, ascites, nausea, vomiting, diarrhea and fever (see Figure 3,).3
Lab findings in lupus enteritis include anemia (52%), leukocytopenia and/or lymphocytopenia (40%), thrombocytopenia (21%) and hypocomplementemia (88%).3
A retrospective study by Koo et al. found C4 was significantly lower in patients with lupus enteritis.1
A retrospective study and systematic literature review by Janssens et al. found the following lab abnormalities in patients with lupus enteritis: ANA (92%), anti-dsDNA (74%), anti-RNP (28%), anti-SSA (26%) and anti-Sm (24%) antibodies, proteinuria >0.5 g/24h (47%), positive antiphospholipid antibodies (30%). Seven patients in this study met criteria for antiphospholipid antibody syndrome.3
In the same review, the authors found the most common radiographic findings were bowel wall edema (91%); double halo or target sign (71%); dilation of bowel lumen (24%); ascites (78%); mesenteric abnormalities (71%), including engorgement of mesenteric vessels; and increased number of viable vessels (comb sign).3
Table 3 shows the frequency of CT findings in SLE patients with undifferentiated acute abdominal pain.6 The jejunum and ileum are more frequently involved, followed by the colon, duodenum and rectum. Of the cases identified in this review, 15% had endoscopy with normal macroscopic findings in 60%.3 Endoscopic biopsy is of low yield. Therefore, lupus enteritis is generally a diagnosis of exclusion.
Table 3: CT Findings of SLE Patients with Undifferentiated Acute Abdominal Pain6
| CT Findings | Frequency (%) |
|---|---|
| Engorgement of mesenteric vessels | 82 |
| Ascites | 77 |
| Bowel wall thickening | 74 |
| Dilation of intestinal segments (5–13 mm) | 74 |
| Comb sign (engorged mesenteric vessels) | 69 |
| Target sign (bowel wall thickening and enhancement) | 66 |
| Retroperitoneal lymphadenopathy | 61.5 |
| Pleural effusion | 33 |
| Splenomegaly | 33 |
| Hepatomegaly | 25.6 |
| Peritoneal enhancement | 23 |
| Hydronephrosis | 23 |
| Lupus nephritis | 23 |
| Lupus cystitis | 15 |
| Pancreatitis | 10 |
| Venous thrombosis | 10 |
| Splenic infarction | 5 |
| Pneumatosis intestinalis | 2.5 |
| Liver abscess | 2.5 |
Treatment
Corticosteroids are the initial treatment for all patients, with an average duration of four days (range 1–34 days).3 Cyclophosphamide can be considered, especially if there is other severe organ involvement (see Figure 4). Maintenance therapy typically includes hydroxychloroquine, mycophenolate mofetil or azathioprine. Most patients have relief of symptoms in less than one week, and recurrence occurs in 23% of patients.3

