
Master1305 / shutterstock.com
We report on a 77-year-old patient who was diagnosed with giant cell arteritis (GCA) on histopathology of the submandibular gland and eventually went on to develop classic signs and symptoms of GCA. This observation highlights neck swelling as a rare initial presentation of GCA.
Case Presentation
A 77-year-old previously healthy man presented to his primary care physician with painless left-sided neck swelling of six months’ duration. Magnetic resonance imaging of the neck demonstrated diffuse homogenous enhancement of the left submandibular gland.
To exclude malignancy, he underwent excisional biopsy of the left submandibular gland, which showed active arteritis with multiple giant cells consistent with GCA, as well as chronic sialadenitis with fibrosis, gland dropout and patchy chronic inflammation, but no evidence of malignancy (see Figure 1). He was referred to a rheumatologist. He denied experiencing symptoms of GCA including headache, jaw claudication, scalp tenderness, fever, fatigue, weight loss, vision changes or polymyalgia rheumatica.
On physical examination, the patient was well appearing, and his temporal artery pulses were equal and without tenderness or nodularity. His erythrocyte sedimentation rate (ESR) was 6 mm/hr (normal: 0–20 mm/hr), his C-reactive protein (CRP) level was <1.0 mg/L, and his hemoglobin and alkaline phosphatase were also unremarkable. A vascular ultrasound of the temporal, subclavian and axillary arteries was normal.
Given the submandibular gland findings, prednisone was recommended for treatment of focal GCA; however, the patient declined treatment and instead remained under close clinical observation with his rheumatologist.
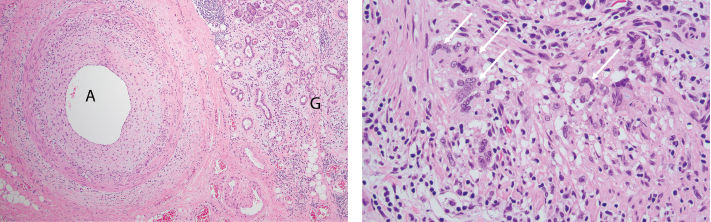
FigureS 1A (left) & 1B: Pathologic Findings of Submandibular Gland Resection
1A) A low-power photomicrograph demonstrates active giant cell arteritis with intimal proliferation and medial chronic inflammation consisting of lymphocytes, macrophages and occasional giant cells within a small artery (A). Chronic sialadenitis manifests as chronic inflammation, fibrosis and gland dropout in the glandular tissue (G). H&E stained section, 40x original magnification.
1B) A high-power photomicrograph demonstrates numerous giant cells (arrows) within the arterial wall. H&E stained section, 200x original magnification.
Eight months later, he developed pain in the right temple, as well as jaw pain with chewing. His ESR and CRP were elevated at 46 mm/hr and 41 mg/L, respectively. Vascular ultrasound was repeated and now showed hypoechoic circumferential wall thickening (i.e., halo sign) in the bilateral axillary arteries consistent with active arteritis in those vessels (see Figure 2). He was started on 40 mg of prednisone daily to treat GCA. His symptoms and inflammatory markers improved, and he was tapered off the prednisone within the subsequent two years without incident.


