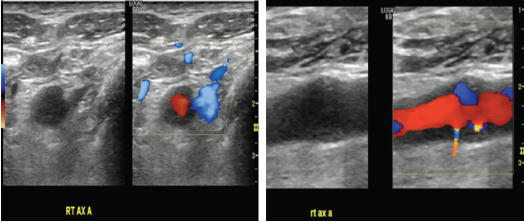
Figures 2a & 2B (from left): Vascular Ultrasound Images
Hypoechoic circumferential wall thickening of the right axillary artery is evident in transverse (A) and longitudinal (B) views.
Discussion
To our knowledge, submandibular swelling as an initial presentation of GCA has been reported only three times in the prior literature.1–3 In two of those cases, diagnosis of GCA was made on the basis of submandibular gland histopathology, as in our patient, and in the third, GCA was diagnosed on temporal artery biopsy. Clinical presentation in these reported cases varied with respect to presence of classic GCA features and inflammatory markers.
Ruiz-Masera et al. reported a case of a 75-year-old woman who presented with a painful right-sided submandibular mass; she had no systemic symptoms of GCA, and her ESR was normal.1 A resection of the submandibular gland mass showed GCA. Five months later, she developed symptoms of systemic GCA with headache, fever, fatigue, arthralgias and elevated ESR, and was treated with steroids.
Förderreuther et al. described a 72-year-old woman who presented with painful periorbital inflammation and submandibular swelling; she lacked other symptoms of GCA, and her ESR was normal.2 A submandibular gland biopsy revealed giant cell arteritis with extension of sclerosing inflammation into the surrounding soft tissue, and she was treated with prednisone and methotrexate.
Finally, Porter et al. reported the case of a 78-year-old woman who presented with several months of right-side submandibular swelling, as well as fever, scalp soreness and an elevated ESR.3 A temporal artery biopsy confirmed the diagnosis of GCA, and prednisone was commenced, leading to regression of the submandibular swelling, although the patient eventually passed away due to intracranial complications of GCA.
In addition to reporting a highly unusual presentation of GCA, our case demonstrates two additional clinical points.
First, branches of the external carotid artery—of which the superficial temporal artery is one—are targeted in GCA. Involvement of other branches of the external carotid system underlies many of the cranial manifestations of GCA (e.g., jaw claudication, facial swelling, dental pain, and pain and unusually overt necrosis of the tongue).4 In our patient, submandibular gland involvement almost surely resulted from arteritis of the gland’s primary blood supply from the submental and sublingual arteries, respectively branches of the facial and lingual arteries, both of which, in turn, are given off by the external carotid artery.
Second, the clinical presentation of GCA can occasionally appear to be clinically isolated, as has been described in the breast, female genitourinary tract and aorta.5–7
Our case underlines the importance of sustained vigilance for the emergence of explicit systemic arteritis, notwithstanding an apparently isolated presentation.


