A punch biopsy of an ulcer from the left lower extremity revealed medium-sized blood vessels in the dermis and dermal-subcutaneous junction, with fibrin deposition in walls, neutrophils, and extravasated neutrophils and erythrocytes in the interstitium (see Figure 2). Histologic features of the skin biopsy were consistent with PAN.
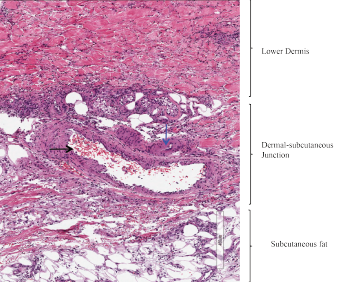
Figure 2: Skin Biopsy
Medium-sized blood vessels are seen in the dermis and at the dermal-subcutaneous junction. The black arrow identifies a venule, and the blue arrow points to a fibrin deposition in the vessel wall. Extravasated neutrophils and erythrocytes are seen in the interstitium.
Treatment with corticosteroids was initiated for the management of cutaneous PAN. The patient reported improvement in the pain caused by his skin lesions; however, his dyspnea, orthopnea and right upper extremity pain persisted.
His chest X-ray suggested low lung volumes (see Figure 3), but computed tomography (CT) of the thorax did not demonstrate parenchymal abnormalities, and CT angiography was unremarkable. Pulmonary function testing revealed a decreased forced vital capacity (FVC) of 33%, forced expiratory volume (FEV1) of 32%, and diffusing capacity for carbon monoxide (DLCO) of 55%, with a normal FEV1/FVC ratio (97).
An electrocardiogram (ECG) showed normal sinus rhythm with borderline left ventricular hypertrophy by criteria. A transthoracic echocardiogram demonstrated a normal ejection fraction with concentric remodeling, and right heart catheterization showed normal filling pressures.
Due to his persistent right arm pain and weakness, the patient underwent electromyography of the right upper extremity. It was suggestive of an inflammatory plexopathy.
We diagnosed PAN with associated shrinking lung syndrome and brachial plexopathy. Shrinking lung syndrome was diagnosed on the basis of the patient’s persistent dyspnea and orthopnea, restrictive pulmonary function tests (PFTs), low lung volumes and a normal CT of the thorax.
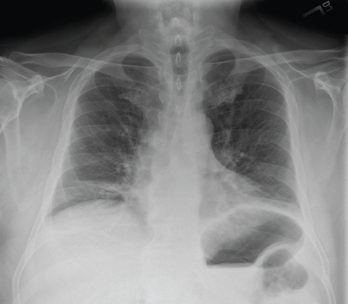
Figure 3: Chest X-ray (Posteroanterior View)
Low lung volumes are appreciated bilaterally, along with subsegmental atelectasis at the right lung base.
The patient was treated with high-dose glucocorticoids, resulting in improvement of his lower extremity ulcers and orchitis. Azathioprine was added as a steroid-sparing agent. Despite improvement in his skin ulcers, he continued to report dyspnea and right arm pain. Azathioprine was changed to methotrexate after he experienced gastrointestinal intolerance. He developed abdominal pain, worsening dyspnea and hyponatremia while on methotrexate, so this medication was discontinued.
More aggressive immunomodulatory therapy with cyclophosphamide was initiated as a result of diaphragmatic weakness and brachial plexopathy attributed to PAN. His clinical course was complicated by hemorrhagic shock, hypoxic respiratory failure and sepsis. Cyclophosphamide was subsequently discontinued. After his recovery and an infection-free interval of a month, he was treated with rituximab for persistent dyspnea. He eventually developed multi-organ failure, which ultimately led to his death.
Discussion
Polyarteritis nodosa is a systemic necrotizing vasculitis that typically affects medium- and small-sized muscular arteries but spares small vessels, such as arterioles, capillaries and venules.1 It is a rare disease that has become even less common with widespread immunization against HBV and better diagnostic criteria for other systemic, necrotizing vasculitides.3
PAN affects men more often than women, with an average age of onset between 40 and 60 years. Constitutional symptoms, such as fever, myalgias and weight loss, along with peripheral neuropathy, are the most common presenting symptoms associated with PAN.1,4 Nearly 60% of patients with generalized PAN develop cutaneous manifestations. About 20% of patients develop orchitis; less commonly, patients may present with gastrointestinal symptoms, including the severe manifestation of an acute abdomen.1,5
Mononeuritis multiplex is the most common neurologic manifestation in PAN and may be present in up to 75% of patients.1 Rarely, brachial or lumbosacral plexopathies, as seen in our patient, have been associated with PAN. Other rare neurologic manifestations include radicular syndromes and a clinical presentation similar to Guillain-Barré syndrome.4


