EMT is a biologic process that allows a polarized epithelial cell, which normally is attached to the basement membrane, to undergo multiple changes that enable it to assume a mesenchymal cell phenotype.5,6 EMT is initiated via inflammation through the activation of transcription factors, expression of specific cell-surface proteins, reorganization and expression of cytoskeletal proteins, production of ECM-degrading enzymes and changes in the expression of specific microRNAs.5,6 The majority of epithelial cells exposed to inflammation undergo apoptosis, but some transition and have enhanced migratory capacity, invasiveness, elevated resistance to apoptosis.5,6 These cells that have undergone EMT have greatly increased production of ECM components after transition.
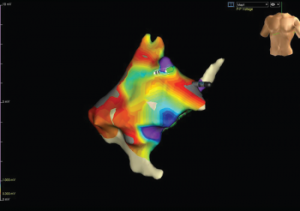
Figure 4: Color Mapping of the Right Atrium
Color mapping is done by electrophysiology to show the amplitude of voltage to evaluate for areas of scarring or fibrosis. Grey areas indicate areas of fibrosis.
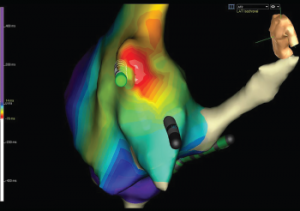
Figure 5: Activation Mapping of the Right Atrium
Activation mapping is done by electrophysiology to evaluate the speed of conduction in the heart. White represents areas of early conduction, which then radiates to slower conduction via change in colors from the spectrum starting with red. The white area is the patient’s re-entrant nidus, and this is the location that the electrophysiologist ablated, resolving the recurrent arrhythmias.
All of these factors, when out of balance with increased deposition of ECM with decreased resorption, result in myocardial fibrosis.5,6 As with the pathophysiology of fibrosis throughout all body tissues in SSc patients, TGF-β via the Smad pathway is one of the key players in cardiac fibrosis as well.3,7
Cardiac complications vary on the basis of the pattern of cardiac fibrosis.4 Patchy fibrosis, in which collagen fibers and myocardial bundles intermingle, is the most proarrhythmic pattern of fibrosis. On the other hand, compact fibrosis is the least proarrhythmic, so when electrophysiologists ablate areas of arrhythmia origination, the goal is to create compact fibrosis to prevent abnormal signal propagation. This is the technique that was successfully completed in our patient’s case.
Conclusion
Understanding the risks of cardiac complications in SSc patients is important for the rheumatologist because cardiac involvement results in increased morbidity and mortality in this patient population.8 In fact, a mere 3% increase in extracellular volume fraction of fibrous tissue in the myocardium is associated with a 50% increase in the risk of adverse cardiac events.9 Keeping in mind that cardiac complications can be subclinical, it is important to risk stratify SSc patients for appropriate screening.
