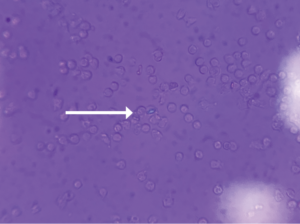
FIGURE 1 (click to enlarge): Intracellular calcium pyrophosphate crystal on polarized light microscopy.
Calcium pyrophosphate crystal deposition disease (CPPD) is an arthritis caused by the accumulation of calcium pyrophosphate crystals. Despite a prevalence of 4–7% among the adult population in Europe and the U.S., it has remained a relatively under-recognized disease owing to its many clinical presentations.1 CPPD may cause an acute mono/oligoarthritis, which may mimic gout or septic arthritis; a chronic arthritis, which may mimic a variety of chronic arthritides (e.g., rheumatoid arthritis, osteoarthritis, ankylosing spondylitis); or a systemic disease, which may mimic sepsis or meningitis. An estimated 25% of initial presentations of CPPD mimic gout or septic arthritis.1 Severity and timing of pain may truly mimic gout, but acute presentations of CPPD are typically less disabling and take longer for pain to reach peak intensity than gouty attacks.2
Although the formal diagnostic criteria have been defined, considerable practical challenges in the diagnosis of CPPD remain. Compared with urate crystals in the context of gout, calcium pyrophosphate crystals are smaller and less birefringent via light microscopy, resulting in less reliability and higher interobserver variability.3
We describe the case of a 78-year-old man with a history of gout who presented with acute-onset unilateral knee pain, initially thought to be due to a septic joint, a condition also known as pseudosepsis, an inflammatory arthritis that cannot be differentiated from septic arthritis on the basis of history, clinical presentation or serum lab values.4
Case Presentation
A 78-year-old man presented to the hospital with a one-day history of severe right knee pain and swelling. He was completely unable to move the knee or bear weight and was brought in via wheelchair. His pain was exacerbated by movement and light touch. He reported an episode of nausea and vomiting just before his arrival that was presumably due to the pain. The patient denied fevers, chills, night sweats, shortness of breath, chest pain, abdominal pain and diarrhea.
The patient’s medical history was significant for gout, myelodysplastic syndrome and stage 3 chronic kidney disease.
His knee was swollen and palpably warm, but without overlying erythema. His range of motion in the knee was limited due to pain. Initial lab tests revealed a C-reactive protein (CRP) of 295 mg/L (reference range [RR]: 0–5.0 mg/L) and a white blood cell (WBC) count of 14.6k/uL (RR: 3.9–10.7k/uL) with neutrophilic predominance. His right knee X-ray revealed mild tricompartmental joint space narrowing with a large joint effusion but no chondrocalcinosis. Arthrocentesis showed 47,628 nucleated cells (92% segmented neutrophils) and 21,000 red blood cells (RBCs) with no crystals seen via light microscopy. Synovial fluid gram stain was was unrevealing and bacterial cultures yielded no growth. Additional 16s and 18s polymerase chain reaction application studies for the detection of bacterial DNA were negative.