High index of suspicion for CPPD is needed in patients older than 65, even in light of other data that may be mistakenly interpreted as evidence of septic joint.
He was immediately taken to the operating room and underwent arthroscopic washout with partial synovectomy. The intraoperative synovial fluid culture failed to yield a culprit organism, although purulent material was noted. After some initial postoperative improvement, his CRP rose to 138 mg/L, prompting an incision and drainage with repeat negative synovial fluid cultures and no bacteria seen in synovial tissue sampling.
He completed a three-week course of antibiotics. However, he remained admitted, with a complex and prolonged hospitalization. Two months later, on hospital day 73, the patient developed acute left knee pain and swelling. Arthrocentesis revealed 42,880 nucleated cells (83% segmented neutrophils), 3,000 RBCs, negative fluid cultures and, once again, no crystals seen via light microscopy. Antibiotics were not initiated at this time given the concern for marrow suppressive effects and the inability to isolate an organism on synovial tissue or fluid culture. He had slow resolution of left knee pain and swelling with conservative pain management.
Three weeks later he had acute worsening of his left knee pain, for which a rheumatologist was consulted. An X-ray of the left knee showed chondrocalcinosis. The serum uric acid level was 8.1 mg/dL (RR: 3.5–7.2 mg/dL). Arthrocentesis revealed 150,927 nucleated cells (90% segmented neutrophils) and 17,000 RBCs. Synovial fluid gram stain and bacterial culture were again negative.
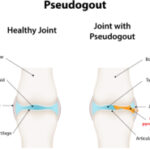
On our manual review of the synovial fluid, positively birefringent crystals were seen with a polarizing microscope within neutrophils, meeting formal criteria for the diagnosis of acute monoarticular CPPD arthropathy (see Figure 1). Anintra-articular steroid injection was performed. Arthrocentesis was repeated two days after the steroid injection, which revealed 80,600 nucleated cells (64% segmented neutrophils) and repeat visualization of CPPD crystals. He completed a three-day course of anakinra and was discharged home on hospital day 94.
Discussion
The differential diagnosis of acute-onset monoarticular joint pain is relatively limited. It may remain a diagnostic challenge, however, in cases where history, physical and serum lab values fail to adequately support or refute a noninfectious vs. an infectious cause—cases aptly termed pseudosepsis.
In addition to CPPD, rheumatoid arthritis, gout, Behçet’s disease, systemic lupus erythematosus, ankylosing spondylitis and psoriatic arthritis have all been reported to present as pseudoseptic arthritis.5 Despite potential fever and leukocytosis, synovial fluid gram stain and culture are repeatedly negative. In one retrospective study across more than two and a half decades at one center, 19% of suspected septic arthritis cases were culture negative.6