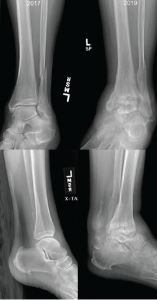
Figure 2: Comparison of X-rays
X-rays from 2017 (left) are notable for preserved joint spaces with distal fibular fracture. The 2019 X-rays (right) show diffuse, soft tissue swelling, severe erosions and talar collapse.
Pertinent lab results at the time of admission included a peripheral leukocytosis of 16.4% (109/L), with 92% neutrophils, erythrocyte sedimentation rate of 25 mm/hr and C-reactive protein of 46.4 mg/L. Arthrocentesis of the left ankle yielded 11,550 nucleated cells (differential not performed) and 25,300 red cells, with a negative gram stain and crystal analysis.
Radiographs demonstrated erosive change of the tibiotalar joints with chronic periosteal reaction and extensive soft tissue swelling, which was significantly changed from X-rays done approximately 19 months earlier (see Figure 2). Magnetic resonance imaging (MRI) showed severe erosive changes, with talar collapse, and complex tibiotalar and subtalar joint effusions, with tenosynovitis of medial flexor tendons and peroneal tendons.
Disseminated sporotrichosis was suspected due to the pattern of destruction in her ankle, as well as the appearance of cutaneous cystic lesions. An MRI of the right forearm was obtained, which demonstrated multiple mildly complex subcutaneous and soft tissue fluid collections, as well as dorsal compartment tenosynovitis (see Figure 3).
The rheumatology team recommended consultation with an orthopedist, who reviewed the imaging and felt the findings were more likely related to sequelae of advanced rheumatoid arthritis than to an atypical infection.
Given the concern for possible disseminated fungal infection and the uncertain etiology of the fluid collections in the wrist, we elected to aspirate the cysts, yielding approximately 10 cc of gelatinous fluid (see Figure 4). The fluid was too viscous for a cell count and differential to be conducted; however, cultures from both the cyst aspirate and the left ankle effusion ultimately grew Sporothrix (see Figure 5).
The patient was started on intravenous amphotericin, as well as oral itraconazole, and underwent incision and drainage of her left ankle and her right forearm lesions. She required multiple surgeries to address chronic left ankle fungal osteomyelitis, with necrosis involving the tibia, fibula and talus.
The infectious disease team recommended ongoing antifungal therapy with itraconazole, with plans for at least one year of treatment after her most recent surgery.
Discussion
Cognitive biases are known to contribute to medical errors and diagnostic delays, and the care of patients with rheumatologic conditions arguably presents an inherently higher risk for these types of errors.1–3 Distinguishing between fungal infections and autoimmune disease can be challenging and requires both careful evaluation and a high degree of suspicion, particularly related to opportunistic infections.
Given that rheumatologic conditions and indolent fungal infections are relatively uncommon, providers may be unfamiliar with possible disease presentations causing a tendency toward search satisfying, in which consideration of alternatives stops once a plausible explanation is found. Wide variation exists in the estimation of infectious risk associated with commonly used rheumatologic therapies, potentially contributing to biased assessment.4
In this case, premature diagnostic closure and confirmation bias likely led the providers to prematurely lock on the known rheumatologic condition and give undue credence to findings that confirmed this diagnosis, excluding data that argued against RA as the sole cause of her illness.5