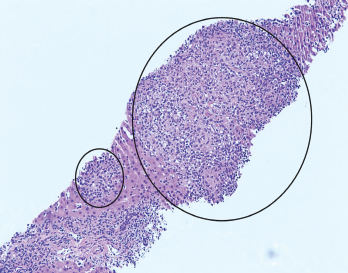
Figure 1. H&E stain at 100X showing granulomas accompanied by scattered admixed lymphocytes.
A 26-year-old woman presented to our emergency department (ED) with intermittent fevers, nausea and vomiting. She had a past medical history of well-controlled, anti-nuclear antibody positive and rheumatoid factor negative polyarticular juvenile idiopathic arthritis (pJIA) and Crohn’s disease. Her maintenance treatment consisted of monthly intravenous infliximab, 10 mg of oral methotrexate weekly and 20 mg of oral leflunomide daily.
The patient had been evaluated two weeks before at an ED in Chicago for sinus congestion and generalized malaise. She reported that a computed tomography (CT) scan of the chest showed “early pneumonia.” She was discharged home with a prescription for azithromycin for a lower respiratory tract infection and told to abstain from her immunosuppressive agents.
Despite completion of the antibiotics, her symptoms worsened. She presented to our ED in Pittsburgh with a temperature of 39.5°C (103.1°F), nausea, vomiting and malaise. On exam, she appeared mildly ill and was tachycardic, with a heart rate of 110–120 beats per minute. The laboratory tests revealed:
- Aspartate aminotransferase (AST) of 486 U/L (RR: 0–32 U/L);
- Alanine aminotransferase (ALT) of 482 U/L (RR: 0–33 U/L); and
- Alkaline phosphatase of 150 U/L (RR: 35–104 U/L).
A chest X-ray did not show active disease.
The patient was given a dose of acetaminophen before the lab results were available, and her fever and tachycardia resolved. Further evaluation in the ED revealed no reactive heterophile antibodies (i.e., monospot test), normal lipase and a PCR test for influenza that was negative. The patient declined admission for further evaluation despite physician recommendations but agreed to return if her symptoms worsened. She was encouraged to keep an outpatient appointment with her primary rheumatologist scheduled for four days later.
The patient returned to the ED two days later with persistent intermittent fevers, nausea and vomiting. She had no headache, and she denied new medications (other than azithromycin), recent medication changes, recreational drug use, over-the-counter supplements, incorrect dosing of current medications or travel outside the U.S. She had been taking methotrexate and leflunomide for 25 and 12 years, respectively. Infliximab infusions had been initiated two years before. Her pJIA and Crohn’s disease were asymptomatic on this treatment regimen, though she had not taken immunosuppressives since onset of the current illness.
On examination, her temperature was 38.5°C (101.3°F), her weight was 74 kg (163 lbs.), and her heart rate was 114 beats per minute. Her general exam was otherwise unremarkable, without focal deficits. Laboratory testing revealed a rising AST of 783 U/L and ALT of 650 U/L, total bilirubin of 1.6 mg/dL (RR: 0.2–1.3 mg/dL), alkaline phosphatase of 195 U/L (RR: 35–104 U/L), platelets of 127,000/mcL (RR: 145,000–445,000 mcL), C-reactive protein of 10.5 mg/dL (RR: <0.5 mg/dL) and erythrocyte sedimentation rate (ESR) of 92 mm/hr (RR: 0–25 mm/hr).
The initial evaluation focused on addressing potential causes of hepatocellular disease. Tests for cytomegalovirus, herpes simplex, Epstein-Barr virus, parvovirus, hepatitis A, B and C, HIV, anti-mitochondrial antibody, anti-smooth muscle antibody, serum copper, ceruloplasmin, alpha-1 antitrypsin level and acetaminophen level were unremarkable.
Ultrasound of her abdomen showed splenomegaly and prominence of periportal fat for which a broad differential was considered, including infectious, medication, metabolic and inflammatory causes. Initial blood cultures demonstrated no growth.
A hepatologist ordered tests for tick-borne diseases and further imaging. Computed tomography (CT) of the abdomen and pelvis showed nonspecific changes of the liver suggestive of hepatitis and partially visualized hilar lymphadenopathy. A liver biopsy was recommended to further evaluate worsening transaminitis.
On the second day of admission, the patient remained febrile. Laboratory tests showed ferritin of 11,806 ng/mL (RR: 6.2–137 ng/mL), a declining absolute neutrophil count of 0.88 k/mcL (RR: 2.0–9.3 k/mcL), platelets of 101 k/mcL, ESR of 25 mm/hr and triglycerides of 298 mg/dL (RR: <150 mg/dL), raising concern for macrophage activation syndrome (MAS).
Intravenous methylprednisolone, 1 g daily, was initiated, with the subsequent addition of 100 mg of subcutaneous anakinra every eight hours.
