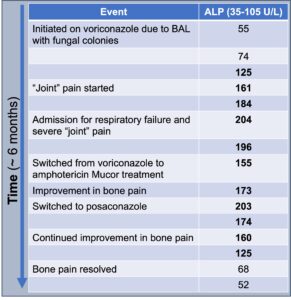
Figure 4
ALP trends over time
Clinically, symptoms of VIP include diffuse, often severe, and constant bone pain that worsens with palpation. In severe cases of periostitis, palpable bony overgrowth and nodules can occur. Joint swelling has been reported, as have non-specific symptoms of myalgias and weakness. The pain tends to be minimally responsive or unresponsive to steroids, colchicine, and opiates. Although any bone can be affected, the ribs, proximal long bones, shoulders and hands are most commonly involved. Excess fluoride can also deposit on dental enamel, resulting in dental fluorosis characterized by white streaks or specks.3,4
Other conditions to consider in a patient with diffuse bone pain include malignancy (particularly leukemia and lymphoma), bone metastasis, multi-focal avascular necrosis, autoimmune inflammatory rheumatic diseases, such as polymyalgia rheumatica, rheumatoid arthritis, osteoarthritis, calcineurin inhibitor-induced pain syndrome and primary pain syndromes, such as fibromyalgia.
The differential diagnosis for periostitis and/or enthesopathic changes includes fluorosis; autoinflammatory bone diseases, such as chronic non- bacterial osteomyelitis; HLA-B27- associated conditions, such as spondyloarthritis or psoriatic arthritis; trauma; infection, such as congenital syphilis; hypertrophic osteoarthropathy; venous stasis-related periosteal reaction; thyroid acropachy; and hypervitaminosis A.2,4,13
Diagnosis of VIP should include: 1) typical symptoms, such as subacute, often severe musculoskeletal pain; 2) compatible radiographic findings on X-ray, computed tomography or bone scan; 3) absence of an alternative diagnosis; and 4) improvement after drug cessation.
Specific laboratory findings can strengthen the diagnosis of VIP. New periosteal bone growth in VIP leads to elevations in ALP and other markers of bone remodeling. Ashmeik et al. found that in patients on voriconazole, an increased average ALP (50 IU/L) was associated with higher odds of incident VIP (odds ratio 1.34 [95% confidence interval 1.11, 1.61], P = 0.002).15 Elevated serum fluoride levels often correlate with symptoms and periostitis, although they are not always present.
Calcium, phosphate, PTH, 25-hydroxy-vitamin D and trough concentrations of voriconazole are typically within normal limits.1,3,4 A retrospective study by Moon et al. found that in patients taking voriconazole who underwent a bone scan and plasma fluoride measurement for skeletal pain, elevated fluoride and ALP levels strongly correlated with periostitis on imaging compared to those without periostitis on imaging (fluoride 12.78 ± 0.96 vs. 3.61 ± 1.29 μmol/L; P < 0.001; ALP 273 ± 35.6 vs. 117 ± 15.7; P = 0.02).14
Radiographic findings of VIP and skeletal fluorosis typically include periosteal thickening, calcification of ligaments, and osteosclerosis. These findings are well-demonstrated on X-ray and bone scan. While magnetic resonance imaging (MRI), CT, single photon emission computed tomography (SPECT/CT), and fluorodeoxyglucose (FDG) positron emission tomography (PET) scans can show abnormalities, these more expensive modalities are generally unnecessary for diagnosing VIP.3,4,11
