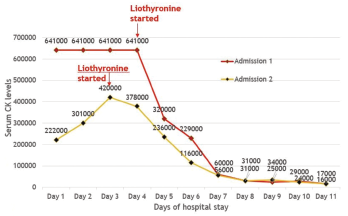
Figure 1: CK Trends During Hospitalization
Rhabdomyolysis is a clinical syndrome characterized by muscle tissue necrosis and release of intramuscular components into the circulation. Typical manifestations include muscle pain and myoglobinuria, causing dark urine. Serum creatinine kinase (CK) enzyme levels are usually markedly elevated. Severity can range from muscle enzyme elevation in the serum of an otherwise asymptomatic patient to extremely high enzyme elevations, causing acute kidney injury, electrolyte imbalance and life-threatening disease with kidney or other organ failure.
We present a case of severe rhabdomyolysis from an unusual cause and associated with much greater CK levels than have been previously reported.
The Case
A 24-year-old African American man came to the hospital with dizziness, dark-colored urine and decreased urine output of four days’ duration. He described increased thirst and had experienced an episode of non-bloody vomiting three days before. He had experienced a few episodes of non-bloody diarrhea six days prior to admission. He smoked marijuana three days prior to symptom onset. He described generalized muscle aches and progressive fatigue. He had no fevers or chills, respiratory symptoms or joint symptoms. Prior to this episode, he’d had no history of exertion or trauma. He was not taking any new medications or using protein supplements. He had never taken a statin.
He had a prior history of congenital panhypopituitarism, diagnosed when he was 2 years old; since that time, he had taken levothyroxine, prednisone and testosterone supplements.
A physical examination revealed tachycardia of 120 beats per minute, but he was otherwise hemodynamically stable. He had normal muscle bulk and tone, and minimal generalized muscle tenderness; his muscle power was 5/5 in all four extremities, as well as in the neck muscles. He had no thyromegaly and no synovitis or rashes.
His laboratory results showed an elevated serum creatinine level of 2.4 mg/dL, and elevated aspartate and alanine transaminase levels of 1,144 and 232 U/L respectively. His CK level was remarkably elevated at 641,820 U/L, and his lactate dehydrogenase level was 10,817 U/L. The markedly elevated CK level was confirmed with repeat analysis, as well as analysis at a different laboratory (see Figure 1).
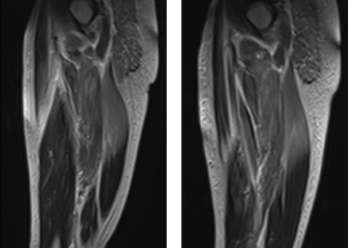
Figure 2: MRI. Magnetic resonance imaging of the bilateral thigh musculature shows extensive increased T2 signal throughout the gluteal musculature, as well as thigh musculature, most prominently in the posterior compartment.
His aldolase level was normal. His inflammatory markers were only minimally elevated, his erythrocyte sedimentation rate was 19 mm/h, and he had a C-reactive protein level of 11.2 mg/dL. His thyroid stimulating hormone (TSH) level was low, at 0.06 mU/L, which was thought to be due to underlying secondary hypothyroidism from panhypopituitarism. His free T4 level was at the lower limit of normal.
Urinalysis showed significant myoglobinuria. Testing for common viral infections causing muscle involvement was negative. His serologies, including anti-nuclear antibodies (ANA), extractable nuclear antigen panel (ENA), myositis-specific and associated antibodies were all negative.
He had experienced a similar constellation of symptoms a year prior, at which time he had severe rhabdomyolysis with a CK level of 82,000 IU/L, which resolved with intravenous (IV) hydration alone and was thought to have an undiagnosed viral etiology.
He reported that his mother also had hypothyroidism and mild systolic heart failure with an ejection fraction of 40%.
The differential diagnosis at this point included: