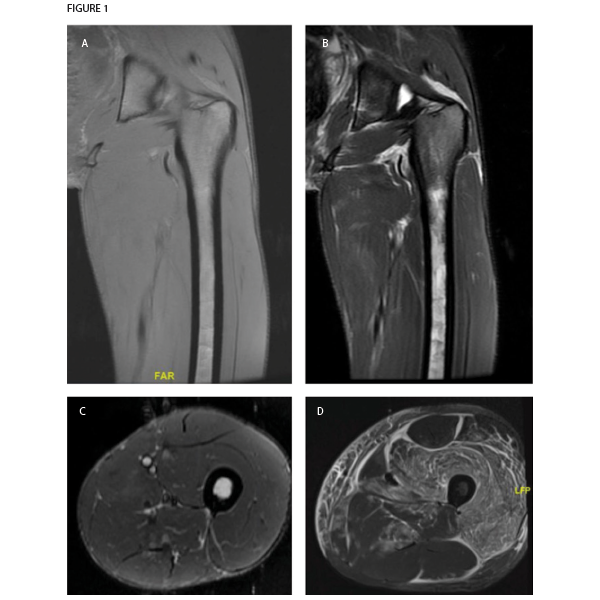
Figure 1. Magnetic resonance imaging of patient’s left thigh. Coronal sections of (A) T1-weighted and (B) T2-weighted sequences both demonstrate extremely thin layer of subcutaneous fat, also seen in the (C) axial section section of STIR sequence imaging. The muscle parenchyma does not have any regions of high T2 signal intensity to suggest muscle edema, as is seen in an axial STIR image from a representative patient with dermatomyositis (image courtesy of Simon Helfgott, MD) (D). The patient’s bone marrow has low T1 and high T2 and STIR signals in the diaphysis of the femur, consistent with serous atrophy. Normal bone marrow has high T1 signal and low T2 and STIR signals.
Our list of differential diagnoses also included occult malignancy, especially in light of the pancytopenia. Lactate dehydrogenase was 182 units/L. The patient refused a bone marrow biopsy. Recent upper and lower endoscopy results were normal. Computed tomography (CT) of the chest, abdomen and pelvis did not suggest malignancy, but was notable for diffuse abnormal appearance of the muscles of the chest, potentially consistent with myositis or myopathy.
An MRI of the thigh was obtained to further characterize the muscle abnormality initially seen in the CT scan. Notably, the muscle parenchyma itself was completely normal, with no signs of edema or fatty replacement. Instead, the MRI revealed a marked decrease in subcutaneous fat. Also, T2 signal hyperintensity was present in the bone marrow of the femur, consistent with serous atrophy. No fractures were seen.
Serous atrophy or gelatinous replacement of the bone marrow is typically seen in situations of starvation, such as cachexia due to malignancy. In younger individuals, it is often caused by anorexia nervosa.1 On MRI, the bone marrow is hypointense on T1-weighted imaging and hyperintense on T2 and STIR sequences, similar to fluid. This unusual pattern of signals is sometimes misinterpreted as a technical problem with the MRI machine, and it is not uncommon for patients to have a second MRI before the diagnosis is made. It does not enhance significantly with contrast, which would instead indicate neoplastic replacement of bone marrow. Patients with serous atrophy of the bone marrow are at high risk of stress fractures (nearly half of patients in one cohort), which can be difficult to detect on MRI due to the hyperintense bone marrow signal.1
When these MRI findings were presented to the patient, he admitted to behavior consistent with an eating disorder, including both deliberate starvation and vigorous exercise. He was referred to psychiatry for treatment.
Discussion
Anorexia nervosa is an eating disorder that predominantly occurs in young women, but can also occur in men. Anorexia nervosa can present with a number of symptoms, signs and even lab results that initially appear consistent with a rheumatologic disorder, including limb pain, weakness, hair loss, rashes, cytopenias and pathologic fractures. For example, leukopenia, anemia and chilblains in a young woman may lead to a referral to rheumatology for consideration of systemic lupus erythematosus. Anorexia nervosa can also cause muscle and bone disease that may prompt evaluation by a rheumatologist.


