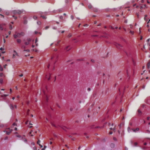
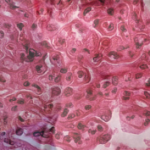
Renal arteriosclerosis is common in patients with lupus nephritis and occurs two decades earlier than it does in people without the condition, say investigators in a study that examined the prevalence of renal arteriosclerosis in patients with lupus nephritis compared with healthy controls.1
The finding suggests that renal arteriosclerosis could be used as a biomarker for early prediction of cardiovascular disease (CVD) risk in patients with lupus nephritis and subsequently lead to timely CVD prevention.
Improving prevention of CVD in patients with lupus nephritis is needed given the high risk of CVD in these patients. Compared with their healthy controls, patients with lupus nephritis have a ninefold higher risk of CVD, according to the researchers. (Note: Another study by Garg et al. presented at the 2019 ACR/ARP Annual Meeting showed that severe renal arteriosclerosis at diagnosis of lupus nephritis increased the risk of CVD tenfold compared with patients without severe renal arteriosclerosis. The study also found a correlation between advanced chronic kidney disease and increased cardiovascular risk in patients with lupus nephritis, with patients with stage 3 or greater chronic kidney disease at a fivefold increased risk of CVD.2 To date, however, biomarkers or tests to predict future CVD are lacking, limiting the ability to identify early who may develop CVD.
Using renal arteriosclerosis as a biomarker or predictor of CVD risk in patients with lupus nephritis is supported by previous studies showing renal arteriosclerosis predicts CVD in other glomerulonephritis diseases, such as IgA nephropathy as well as in renal transplant patients.3-5 Until now, however, no studies have shown a positive association between the presence of renal arteriosclerosis and CVD occurrence in patients with lupus nephritis.
One reason may be the lack of emphasis in the current International Society of Nephrology/Renal Pathology Society (ISN/RPS) guidelines on universal reporting using standard criteria for renal arterial changes, according to Shivani Garg, MD, MS, assistant professor of medicine, Division of Rheumatology, University of Wisconsin, Madison.
The study bore this out. Garg et al. also looked at whether renal arteriosclerosis and its severity were under-reported in pathology reports of patients with lupus nephritis and found they were overlooked or missed in >50% of the pathology reports reviewed.
“Clinicians urgently need early predictors of CVD in patients with lupus nephritis to prevent related morbidity and mortality,” state the authors in the study. “Renal arteriosclerosis on pathology reports could be an early predictor of CVD in patients [with lupus nephritis].”