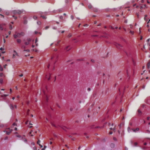
When comparing these readings to the original pathology reports, the investigators found that >50% of the original reports missed renal arteriosclerosis and nearly 40% lacked details on arteriosclerosis or arterial changes.
Although the positive predictive value of the routine pathology reporting was 80% in the study, the over-read analysis using the Banff criteria showed that the assessment of arteriosclerosis in lupus nephritis biopsies is under-reported.
“Our study underscores a need for universal use of systemic Banff renal arteriosclerosis grading criteria in all lupus nephritis biopsies, similar to transplant pathology reporting standards,” says Dr. Garg.
Dr. Singh believes more emphasis will now be placed on looking for renal arteriosclerosis in patients with lupus nephritis, given the findings of the study. He urges clinicians to ask pathologists to comment on the presence or absence of renal arteriosclerosis when examining kidney biopsies from patients with lupus nephritis.
“The increased awareness that the presence of arteriosclerosis in kidney biopsies from patients with lupus nephritis predicts future development of cardiovascular disease will lead to increased reporting of arteriosclerosis on kidney biopsies,” predicts Dr. Singh.
Mary Beth Nierengarten is a freelance medical journalist based in Minneapolis.
References
- Garg S, Bartels CM, Hansen KE, et al. High burden of premature arteriosclerosis on renal biopsies in incidence lupus nephritis. Arthritis Care Res (Hoboken). 2020 Jan 7. doi: 10.1002/ acr.24138. [Epub ahead of print]
- Garg S, Panzer S, Hansen K, et al. Renal arteriosclerosis predicts cardiovascular disease in lupus nephritis [abstract 1564]. Arthritis Rheumatol. 2019;71(suppl 10).
- Myllymäki J, Syrjänen J, Helin H, et al. Vascular diseases and their risk factors in IgA nephropathy. Nephrol Dial Transplant. 2006;21(7):1876–1882.
- Myllymäki J, Honkanen T, Syrjänen J, et al. Uric acid correlates with the severity of histopathological parameters in IgA nephropathy. Nephrol Dial Transplant. 2005;20(1):89–95.
- Loupy A, Vernerey D, Viglietti D, et al. Determinants and outcomes of accelerated arteriosclerosis: Major impact of circulating antibodies. Circ Res. 2015;117(5):470–482.
Previously published in The Rheumatologist in February 2021.