In a clinical pathologic conference presented in the New England Journal of Medicine (NEJM) in 2011, a brain biopsy in a patient with Susac’s syndrome was performed. Findings demonstrated swollen endothelial cells, a small amount of mononuclear-cell perivascular inflammation, and intraluminal hyaline thrombi, suggestive of a microangiopathy.11 There was no evidence of granulomatous angiitis, demyelination, malignancy, or infection. In other cases, brain biopsy has revealed both acute and subacute microinfarcts, and changes in the microvasculature, similar to the NEJM case.11-14
MRI findings in Susac’s syndrome include small, multifocal T2 hyperintensities, most notably in the cerebral white matter and the corpus callosum, and approximately 30% have leptomeningeal enhancement.15 Lesions are hyperintense on FLAIR images. All of the reported cases involve the corpus callosum, usually the central fibers, but spare the periphery, which is distinct from the MRI findings in patients with MS or ADEM.6 This feature was also seen in our patient. Given the small size of the vessels involved, MRA and standard cerebral angiography are normal in patients with Susac’s syndrome. EEG findings are nonspecific.
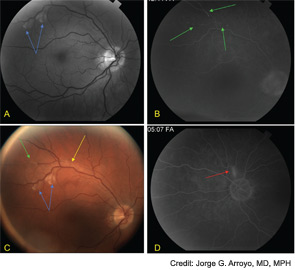
Fluorescein angiography of the retina often shows hyperfluorescence of the wall of the retinal arterioles, and complete occlusion of distal branches.16 The occlusions may be associated with Gass plaques, atheromatous deposits caused by leakage of lipids into the arterial wall at the site of damage.16 Cotton wool patches and boxcar segmentation may also be seen, as was seen in our patient. Pathologic analysis of the retina have demonstrated serous deposits, with compression of retinal vessel lumens, no thrombosis, and decreased adenosine diphosphatase (ADPase) activity suggesting endothelial cell dysfunction and vaso-occlusion.17 Patients do not have visual loss when the occlusions spare the macula.
Susac’s syndrome also includes sensorineural hearing loss, usually of low to mid-frequency, which can be insidious in onset, and either unilateral or bilateral.18 It is sometimes associated with ataxia, vertigo, and nausea, consistent with symptoms experienced by our patient. SG is currently awaiting audiologic evaluation to confirm physical examination findings of right-sided hearing loss.
The clinical course of Susac’s syndrome tends to be self-limited, but can recur, and varies in duration from six months to five years.16 Approximately 60% to 70% of patients experience some degree of persistent encephalopathy, which may manifest as psychiatric disturbances or dementia.6,9,16 The prognosis for recovery of hearing is variable, with some persistence of hearing loss but with improvement in tinnitus and vertigo.19 Visual loss recovery depends on the areas of the retina involved.

