In another study among multiple myeloma patients treated with zoledronic acid or pamidronate, the authors found 10 known SNPs involved in bone turnover associated with MRONJ.30 The genes included COL1A1, CYP2C8, MMP2, OPG, OPN, RANK and TNF.31
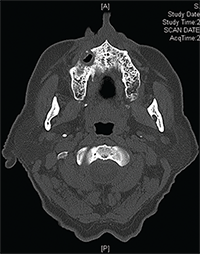
Figures 3A & B: Maxilla involved by osteonecrosis: (top) necrotic bone of right maxilla; and (bottom) bone defect of right maxilla with maxillary sinus involvement.
Another genome-wide association study showed that individuals with an SNP in the RBMS3 gene (associated with collagen formation and bone density) were approximately six times more likely to develop MRONJ.32
Prevalence
Bisphosphonate use is associated with MRONJ in both patients on cancer therapy (frequency of 1–7%) and those with osteoporosis (frequency of 0.02%).33,34 Denosumab use has also been associated with the development of MRONJ in patients with cancer at a frequency of 0.7–1.9%.35 In patients who received denosumab for osteoporosis, the risk for MRONJ is significantly lower (0.04%).36
The risk for MRONJ in patients with cancer on bevacizumab is 0.2%, and increases to 0.9% when used in combination with bisphosphonates.23 There are only a few case reports of MRONJ developing in patients with metastatic renal cell carcinoma treated with sunitinib with no exposure to bisphosphonate therapy.25,26,37
However, the incidence may be as high as 29% in patients with renal cell carcinoma treated with both sunitinib and zoledronic acid.38 Finally, MRONJ has been noted in 1.4% of patients on cabozantinib (a TKI with anti-VEGF receptor) for treatment of metastatic medullary thyroid cancer.39,40
Risk Factors
The single most important risk factor for MRONJ is the cumulative dose of bisphosphonate (because of its long half-life) and, therefore, to some extent, the duration of therapy. In patients with cancer exposed to zoledronic acid or denosumab, the incidence of developing MRONJ increases over time (0.6% and 0.5% at one year, 0.9% and 1.1% at two years, and 1.3% and 1.1% at three years).41 Intravenous zoledronic acid is associated with a higher risk, but this is likely because this is primarily used in cancer therapy and dosed monthly (4 mg) at least for the first two years, and IV bisphosphonate use in osteoporosis is dosed annually, although at a 25% higher dose (5 mg).42,43 As such, duration of use is not as accurate a measure of risk as total cumulative dose.
The other very important risk factor is local trauma, such as from dento-alveolar surgery (e.g., dental extractions), physiologic trauma especially from anatomic factors, such as protuberant tori, and exostoses, although some cases are idiopathic. MRONJ following a tooth extraction in patients with cancer or Paget disease receiving IV bisphosphonates is less than 1%.44 For patients receiving oral bisphosphonates, the risk of ONJ after a dental extraction is 0.09–0.34%.45 In some cases, extractions expose a preexisting site of bone necrosis that caused the tooth to be painful and loose.


