Systemic lupus erythematosus (SLE) can present in many ways and can be difficult to diagnose. Its association with celiac sprue has been only rarely documented, but has appeared in several case reports. When presenting together, it can be difficult to distinguish the underlying disease, because SLE itself has been known to cause malabsorption.
This case report reflects the diagnostic challenges we faced during one patient’s long, complicated hospitalization.
The Case
A 25-year-old, previously healthy, white male presented to our hospital with fever, cough, nausea and vomiting of several weeks duration. He reported a 35 lb. weight loss over the previous year and had recently developed painful oral ulcers. Roughly three weeks prior to admission, he had seen a gastroenterologist for these complaints and was found to have anti-tissue transglutaminase IgA antibodies (anti-TGA IgA) consistent with a diagnosis of celiac disease.
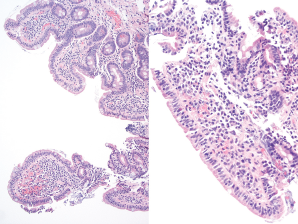
Figure 1. Duodenum biopsy showing partial villous atrophy with borderline increase in intraepithelial lymphoctyes.
An esophagogastroduodenoscopy was performed on an outpatient basis, with findings that could be compatible with malabsorption, possibly due to celiac sprue (see Figure 1). He refrained from eating gluten and his symptoms improved.
He was also undergoing an outpatient evaluation for mild pancytopenia.
At the time of admission, his complete blood count showed the following: white blood cell count 1.9/µL, hemoglobin 12.1 g/DL, and platelets 119 µL. He was found to have an aspartate aminotransferase of 244 (IU)/L and an alanine aminotransferase of 341 (IU)/L. Additionally, he had anti-smooth muscle antibodies, which prompted a liver biopsy that showed only mild steatosis. The consulting hepatologist felt it could be related to his recent diagnosis of celiac disease.
Rheumatology was consulted two days into his hospitalization. He had joint pain in his hands with less than 10 minutes of morning stiffness. On exam, he had dry mucous membranes with three oral ulcers present on the hard palate and a faint red rash on his nose and palms. His breath sounds were minimally decreased without rales or rhonchi. Musculoskeletal exam showed mild synovial thickening of the third proximal interphalangeal joints bilaterally. He was noted to have anti-nuclear antibodies, with a titer of 1:640, in a homogenous pattern. His laboratory tests were also remarkable for a low C3 and C4, and an anti-cardiolipin IgG, which was deemed to be moderately positive. His serum protein electrophoresis was significant for only non-specific hypergammaglobulinemia. His anti-Ro, anti-La, anti-Smith, anti-ribonuclear protein, beta-2 glycoprotein and lupus anticoagulant tests were all negative. During that time, he was mildly hypoxic, and complained of a cough but not dyspnea.