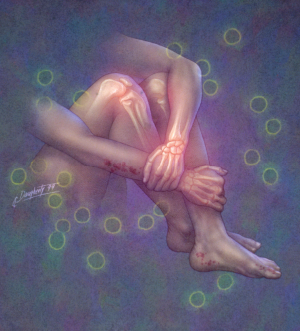
John M. Daugherty/Science Source
WASHINGTON, D.C.—A new, humanized anti-BDCA2 monoclonal antibody can trigger inhibition of the production of interferon, cytokines and chemokines derived from plasmacytoid dendritic cells in patients with cutaneous systemic lupus erythematosus (SLE), according to research presented at the 2016 ACR/ARHP Annual Meeting.
The findings were discussed during a session on SLE treatment, drug adherence and the effects of the monoclonal antibody anifrolumab. Experts at the session, Systemic Lupus Erythematosus—Clinical Aspects and Treatment III: Novel and Current Therapies, told attendees that circulating plasmacytoid dendritic cells, the major producers of type 1 interferons, are decreased in lupus, but found in greater numbers in organs affected by the disease. BDCA2 is an inhibitory receptor expressed exclusively on these cells.
In a phase 1 study, researchers enrolled 12 patients with acute, subacute or chronic cutaneous lupus.1 Eight patients received the drug, BIIB059, and four controls received placebo. Researchers found that those who received single doses of the antibody, at 20 mg/kg, had a dampened expression of interferon-responsive genes in the blood and interferon-responsive proteins in the skin, said Richard Furie, MD, the principal investigator and professor of medicine at Hofstra Northwell School of Medicine in Long Island, New York.
In comparison to one in four patients in the placebo group, six of the eight patients who received treatment had at least a four-point reduction in their Cutaneous Lupus Erythematosus Disease Activity and Severity Index (CLASI) score from baseline at Week 4 or Week 12. But Dr. Furie said the patient in the placebo group who responded had a much higher CLASI than the rest of the patient pool at baseline and also received steroids, which could have accounted for the response.
Skin biopsies were evaluated at baseline and at Week 4 for interferon-regulated proteins, and researchers found that an improvement in CLASI scores correlated with a reduction in myxovirus-resistance protein 1, a protein associated with activation of the interferon pathway. The correlation coefficient was 0.78.
Adverse events were balanced between placebo and treatment arms, with only one serious adverse event, which was not related to the drug. No patients withdrew due to adverse events.
“We did see benefit to some patients and the Phase 2 study is just about to start,” Dr. Furie said.
Impact of Nonadherence Studied
Experts also discussed a separate prospective study conducted at 19 centers across 10 countries in Europe and whose findings show the importance of using multiple ways to assess nonadherence to medication among patients with SLE.2
The 305 patients who were enrolled—all of whom had been prescribed hydroxychloroquine (HCQ) at least two months before and were having a disease flare, according to the SELENA-SLEDAI Flare Index—had their HCQ blood levels tested; answered the Medication Adherence Self-Report Inventory questionnaire; and were assessed for drug adherence by a physician using the Visual Analogue Scale.
Blood tests revealed that 18.5% of patients were severely nonadherent; they had less than 200 mg/mL in their system or undetectable levels of desethylchloroquine (DCQ) (a metabolite of HCQ), which suggested they only very recently had resumed treatment.
About 40% of patients were found to be nonadherent using the questionnaire. Some patients with undetectable HCQ and DCQ still had questionnaire scores of 80%, which suggested to researchers that some patients were reluctant to admit severe nonadherence, perhaps even to themselves.
The researchers determined that 40.3% of patients were nonadherent, defined as taking less than 80% of their HCQ in the previous month. Younger age and the absence of steroid use were predictors of nonadherence, whether it was determined by blood levels, questionnaire answers or physician assessment, the researchers found.
“Nonadherence can be missed by the physician and underreported by the patient, strongly suggesting the usefulness of blood assays in this setting and the value of using different methods to increase the likelihood of diagnosing nonadherence,” said Nathalie Costedoat-Chalumeau, MD, PhD, professor of internal medicine at Cochin University Hospital in Paris, who presented the findings.
Researchers also presented findings that detailed the effects of anifrolumab, an antibody that targets the type 1 interferon receptor, on specific symptoms experienced by patients with SLE.3 The drug was found safe and effective overall in the phase 2 MUSE trial, results of which were also presented at the ACR/ARHP Annual Meeting. About 300 patients with moderate to severe active SLE received either 300 mg or 1,000 mg of anifrolumab, or placebo, every four weeks.
The current report broke this down to individual symptoms of rash, alopecia and arthritis. Patients with high interferon signals had significant improvements in rash, alopecia and arthritis with the best results for the patients on the 300 mg dose.
“Single-organ assessments showing a range of effects on arthritis and skin worked well to demonstrate the treatment effect,” said Joan Merrill, MD, of the Oklahoma Medical Research Foundation in Oklahoma City. “These data contribute understanding of the impact of anifrolumab on individual lupus features and suggest benefits of continuous variables in outcome measures to inform interpretable trial designs.”
Thomas R. Collins is a freelance writer living in South Florida.
References
- Furie R, Werth V, Merola J, et al. BIIB059, a monoclonal antibody targeting BDCA2, shows evidence of biological activity and early clinical proof on concept in subjects with active cutaneous SLE [abstract 2013]. Arthritis Rheumatol. 2016;68(suppl 10).
- Costedoat-Chalumeau N, Houssiau F, Izmirly P, et al. Predictive factors of adherence to treatment in an international prospective study of blood hydroxychloroquine levels in SLE patients with flares [abstract 2010]. Arthritis Rheumatol. 2016;68(suppl 10).
- Merrill J, Furie R, Werth V, et al. The effect of anifrolumab on cutaneous manifestations and arthritis in moderate to severe systemic lupus erythematosus (SLE) using categorical SLEDAI-2K responses and continuous measures of activity as outcome measures [abstract 2009]. Arthritis Rheumatol. 2016;68(suppl 10).


