Over 50% of patients with systemic sclerosis (SSc) develop interstitial lung disease (ILD), and rheumatologists have long recognized this major cause of morbidity and mortality.1 Sindhu R. Johnson, MD, PhD, professor of medicine at the University of Toronto, Canada, and director of the Toronto Scleroderma Program, notes that more recent studies have increased our awareness of the risks for ILD in other systemic autoimmune rheumatic diseases (SARDs), such as rheumatoid arthritis and Sjögren’s disease. Although comparatively lower than in SSc, the incidence of ILD in these diseases is still significant.
Over 50% of patients with systemic sclerosis (SSc) develop interstitial lung disease (ILD), and rheumatologists have long recognized this major cause of morbidity and mortality.1 Sindhu R. Johnson, MD, PhD, professor of medicine at the University of Toronto, Canada, and director of the Toronto Scleroderma Program, notes that more recent studies have increased our awareness of the risks for ILD in other systemic autoimmune rheumatic diseases (SARDs), such as rheumatoid arthritis and Sjögren’s disease. Although comparatively lower than in SSc, the incidence of ILD in these diseases is still significant.
Clinicians now have guidelines to refer to regarding the screening, monitoring and treatment of patients with ILD secondary to SARDs. The guidelines will help clinicians quickly diagnose and optimally manage these diseases.1,2
In January, The Rheumatologist, the ACR and Wiley presented a webinar featuring the following speakers: Dr. Johnson, principal investigator for the guidelines, and Elana J. Bernstein, MD, MSc, Florence Irving associate professor of medicine in the Division of Rheumatology at Columbia University, New York City, and co-first author of the guidelines.
Background
When it occurs in the context of a SARD, progression of ILD varies widely. It can present with subclinical features, such as mild cough, following a slow, progressive course, or with more acute manifestations and rapid disease progression with severe deterioration of pulmonary function. Alveolitis from activated T cells can result in the release of cytokines and the accumulation of alveolar macrophages, T lymphocytes and neutrophils in the lungs. Ongoing inflammation can lead to tissue injury and, sometimes, eventually fibrosis, which may be progressive.3
 Immunosuppressants are the cornerstone of therapy for SARD-ILD, according to Dr. Bernstein, because they address ongoing inflammation. In the webinar, she discussed how the guidelines were developed. Like other recent ACR guidelines, these rely on the GRADE methodology (Grading of Recommendations, Assessment, Development and Evaluation) to rate the certainty of evidence on the basis of a literature review targeted to specific, clinically relevant PICO (i.e., population, intervention, comparator and outcome) questions. A panel that included both clinicians and patients voted on the final recommendations.
Immunosuppressants are the cornerstone of therapy for SARD-ILD, according to Dr. Bernstein, because they address ongoing inflammation. In the webinar, she discussed how the guidelines were developed. Like other recent ACR guidelines, these rely on the GRADE methodology (Grading of Recommendations, Assessment, Development and Evaluation) to rate the certainty of evidence on the basis of a literature review targeted to specific, clinically relevant PICO (i.e., population, intervention, comparator and outcome) questions. A panel that included both clinicians and patients voted on the final recommendations.
These recommendations are meant to guide shared decision making between clinicians and patients, and should not be used by third parties to constrain diagnostic or treatment options, says Dr. Bernstein.
The guidelines and recommendations apply specifically to adult patients with systemic sclerosis, idiopathic inflammatory myopathies, mixed connective tissue disease, rheumatoid arthritis or Sjögren’s disease.
Screening & Monitoring for ILD
To help with screening decisions, the first guideline provides a detailed list of disease-specific factors that may increase a patient’s risk of developing ILD, drawing on elements from a patient’s medical history, current presentation and laboratory results.1 Patients who lack the risk factors and are asymptomatic may not necessarily need screening beyond their regular history and physical exam (see Figure 1).
“If clinicians are uncertain whether a patient should be screened or not, they should err on the side of caution and screen,” says Dr. Johnson.
One recommendation: Pulmonary function tests (PFTs) are conditionally recommended over history and physical exam or ambulatory desaturation testing alone to screen for ILD in SARD patients at higher risk.
Others conditional recommendations are for high-resolution computed tomography (HRCT) of the chest over PFTs alone, and for HRCT over history and physical exam, as well as in favor of chest HRCT with PFTs over PFTs alone.
Dr. Bernstein has a strong preference for screening all people who have SSc with HRCT at presentation, due to the high prevalence of the disease in this population and the fact that PFTs alone may miss early ILD.
The Patient Panel expressed a strong preference for early diagnosis of ILD, even if more frequent screening leads to identification of subclinical disease or incidental findings that may require further testing.
Once diagnosed with ILD, SARD patients require monitoring for their response to therapy, typically in conjunction with pulmonology. The Patient Panel strongly preferred more frequent testing over less frequent testing to avoid missing signs of progression.
Treatment of ILD in SARDs
Most recommendations in the treatment guideline were based on low or very low certainty of evidence, as were the recommendations on screening and monitoring treatment. Dr. Johnson points out that in these circumstances, patients’ preferences and values more strongly influence treatment choice. “The Patient Panel told us they wanted clear communication about the advantages and side effects [of therapies], so they could be actively involved in their choice of medication,” she says.
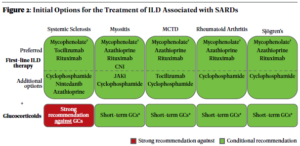
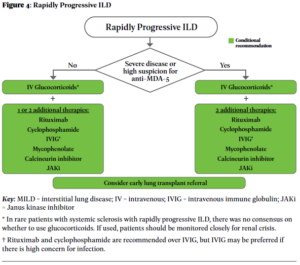
The guideline recommendations are stratified by first-line treatments (see Figure 2) vs. treatments to consider if a patient’s disease has progressed after initial treatment, with certain recommendations specific to individual SARDs (see Figure 3). Additional recommendations clarify additional treatment approaches in patients with rapidly progressing disease (see Figure 4).
Glucocorticoids
Recommendations: A strong recommendation against glucocorticoid use in patients with SSc as first-line treatment of SARD-ILD was made. However, for patients with ILD related to other SARDs, the conditional recommendation is in favor of glucocorticoid treatment in conjunction with another therapy, usually a traditional immunosuppressive.
The strong recommendation against glucocorticoids as first-line ILD treatment in systemic sclerosis, one of the few strong recommendations in the guideline, is due to the risk of inducing renal crisis in this population. “I think rheumatologists are very familiar with this risk, but people outside the rheumatology community [may] be less so,” says Dr. Bernstein.
In all likelihood, notes Dr. Johnson, clinicians should also avoid glucocorticoids in patients with mixed connective tissue disease who have a scleroderma-dominant phenotype.
Immunomodulators: Initial Treatment
Recommendations: Mycophenolate, rituximab, cyclophosphamide and azathioprine are conditionally recommended as first-line treatments for SARD-ILD, with mycophenolate conditionally recommended above these other agents.
Dr. Johnson notes that guideline developers preferred some agents due to published literature and expert experience, but other agents may be options in specific circumstances. Thus, although these are all potential first-line options, cyclophosphamide and azathioprine may be considered additional options rather than preferred first-line treatment.
In this webinar presented by The Rheumatologist, the ACR and Wiley, Dr. Johnson and Dr. Bernstein discuss the development of the guidelines and the recommendations they contain. Click the image to watch the webinar recording.
Dr. Bernstein notes that many physicians may be reluctant to prescribe cyclophosphamide due to concerns of infection, hemorrhagic cystitis and potential infertility; mycophenolate has a comparatively better side effect profile.
See the full guidelines for additional recommendations with respect to treatment after progression, use of antifibrotics and additional therapies, as well as considerations in rapidly progressing disease.
Ruth Jessen Hickman, MD, a graduate of the Indiana University School of Medicine, is a medical and science writer in Bloomington, Ind.
References
- Johnson SR, Bernstein EJ, Bolster MB, et al. 2023 American College of Rheumatology (ACR)/American College of Chest Physicians (CHEST) guideline for the screening and monitoring of interstitial lung disease in people with systemic autoimmune rheumatic diseases. Arthritis Rheumatol. 2024.
- Johnson SR, Bernstein EJ, Bolster MB, et al. 2023 American College of Rheumatology/American College of Chest Physicians (CHEST) guideline for the treatment of interstitial lung disease in people with systemic autoimmune rheumatic diseases. Arthritis Rheumatol. 2024.
- van den Bosch L, Luppi F, Ferrara G, Mura M. Immunomodulatory treatment of interstitial lung disease. Ther Adv Respir Dis. 2022;16:17534666221117002.
Adapted from an article in the August 2024 issue of The Rheumatologist (Vol. 18, No. 8).