A brain CT and an MRI (see Figure 1) were not consistent with a stroke. He was diagnosed with possible posterior reversible encephalopathy syndrome (PRES) and was discharged to a rehabilitation facility for physical and occupational therapy.
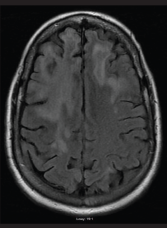
FIGURE 1: An MRI of the brain performed without contrast on June 25, 2016, showed extensive and nonspecific signal abnormalities in the cortical ribbon and subcortical white matter of the right frontal lobe. There is minimal associated parenchymal atrophy in this region without evident edema. No pathologic enhancement, diffusion restriction nor hemosiderin deposition were associated with such signal abnormality.
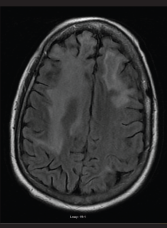
FIGURE 2: An MRI of the brain performed without contrast on July 7, 2016, showed persistent abnormalities in the frontal lobes, which in the right extended into the anterior adjacent parietal lobe. The abnormalities were greater in the right lobe than in the left. Findings in the occipital lobes did not have convincing evidence of restricted diffusion or hemorrhage.
He continued to deteriorate neurologically, which prompted a second neurology consultation. A repeat MRI (see Figure 2) and lumbar puncture were done (see Table 2). Electroencephalogram (EEG) was conducted and was consistent with mild encephalopathy. Laboratory data (see Table 2) supported a hypogammaglobulinemia with low IgG and IgM. IgA was within the normal range. CD4 and CD8 values were low. Cerebral spinal fluid (CSF) results were fairly bland, with the exception of a mild increase in RBCs. Further CSF studies, which were normal, included VDRL, EBV and oligoclonal bands. Cytology of the CSF demonstrated mature lymphocytes without malignant cells present. The CSF did demonstrate a significant elevation in myelin basic protein with a positive PCR for the JC virus.
Our patient was diagnosed with PML based on the above findings. Unfortunately, there are no FDA-approved treatment modalities for this disease process. We discussed potential experimental treatment options with the patient, but we agreed on palliative care alone.
Aggressive physical and occupational therapy were continued, and the patient was discharged home with hospice. He passed away a few months after the initial diagnosis was made.
Discussion
Progressive multifocal leukoencephalopathy (PML) is a rare, fatal, demyelinating disease of the CNS caused by lytic replication of the John Cunningham (JC) virus. The JC virus is ubiquitous in the human body and has an estimated prevalence of 40–70% in the general population.1 The JC virus is usually kept in check by the healthy immune system. However, in the right setting, the virus will invade the CNS and cause an untreatable disease state. The transformation from benign bystander to deadly disease is facilitated by an immunocompromised host, either by infection with the human immunodeficiency virus (HIV) or by immunosuppressive drugs.
