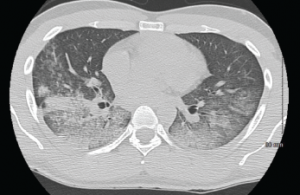
A CT scan of the chest showing multifocal ground-glass opacities, representative of hemorrhage, with numerous nodular interstitial opacities primarily within a peribronchovascular distribution.
A 22-year-old Indian male presented to the emergency department with hemoptysis. A month prior, he had presented to an urgent care center complaining of cough with occasional episodes of blood-tinged sputum in the morning. He was diagnosed with community-acquired pneumonia based on a chest X-ray without laboratory testing and was prescribed levofloxacin.
A few days later, he called his primary care physician for bilateral ankle pain and was told that this could be due to fluoroquinolone-induced tendinitis. The ankle pain, as well as his cough, varied in intensity before he presented to the hospital, and during this interval he also noted bilateral knee, wrist and right elbow pain. He also noted that his eyes had been “bloodshot” recently, but denied visual changes or eye pain.
The day prior to his presentation at our hospital, he noted an acute worsening of his cough with more frequent hemoptysis and new dyspnea. His primary care physician ordered a chest X-ray that was suggestive of worsening multifocal pneumonia.
On admission, the patient did not report any fevers, weight loss, night sweats, rash, dysuria, bloody stools, diarrhea or lymphadenopathy. He denied sexual activity, smoking and illicit drug use. He was not taking any medications other than acetaminophen and ibuprofen as needed. His only travel had been to Texas a year earlier for mountain climbing, and he denied any recent sick contacts or any incarceration.
His vitals: blood pressure 114/84 mmHg; heart rate 116 beats/minute; temperature 97.5º F; respiratory rate 16 per minute; oxygen saturation 90% on room air, which improved to 98% on 2L O2 via nasal cannula. His complete blood count revealed a hemoglobin of 9.9 g/dL, WBC of 10,000 without bands, platelets of 301,000. His electrolytes, as well as renal and hepatic function, were within normal limits. ESR and CRP were 82 mm/hr and 144 mg/dL, respectively. Urinalysis was notable for 2+ blood with 11–20 RBCs/hpf without casts. A chest X-ray showed multifocal opacities, most pronounced in the right upper lobe. The cardiopulmonary exam was significant for tachycardia, with regular rhythm and bilateral rales. Bilateral conjunctival injection was noted, with a normal nasopharyngeal exam. The musculoskeletal exam revealed periarticular tenderness of the knees and wrists bilaterally, and pain with active and passive flexion of the right elbow, and tenderness to palpation of the right posterior ankle. No rash was visualized.


