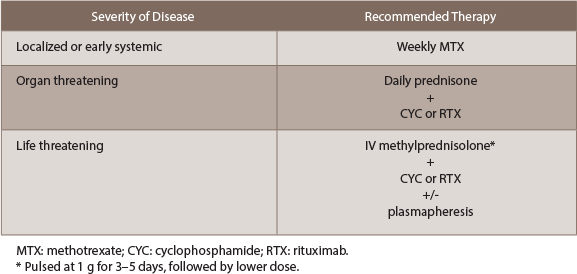
For disease that is organ threatening, daily prednisone with the addition of either cyclophosphamide (CYC) or rituximab (RTX) is recommended. This recommendation is based on the RAVE trial, which found RTX to be noninferior to CYC. CYC can be given as either a monthly IV pulse or a daily dose, the latter offering less risk for relapse at the expense of side effects.8 With CYC, the absolute neutrophil count should be kept >1000/μL. Rituximab can be given as a weekly dose of 375 mg/m2 over four weeks or a 1,000 mg biweekly dose over two weeks. Before starting rituximab, it is imperative to test patients for hepatitis B and tuberculosis.
Patients with life-threatening disease benefit from the addition of plasmapheresis to dual corticosteroid and CYC/rituximab therapy (see MEPEX trial9). Intravenous methylprednisolone should be started immediately, at a pulse dose of 1 gram for three to five days, followed by a lower dose. If a patient is receiving both rituximab and plasmapheresis, it’s important to perform plasmapheresis first, because a portion of rituximab will be removed. The major indications for plasmapheresis are: 1) advanced kidney disease (requiring hemodialysis, creatinine >4 mg/dL or rapidly declining function); 2) positive anti-GBM antibodies; and 3) pulmonary hemorrhage.8
Maintenance therapy: Once remission is achieved, the goal is to step down therapy to medications that are less toxic. If remission is not reached within six months, this should be considered as induction failure and the regimen should be changed; for example, the RAVE trial found rituximab was superior to CYC in relapsing AAV.9 The typical maintenance regimen typically consists for low-dose prednisone in combination with another immunosuppressant, such as azathioprine (AZT), methotrexate, mycophenolate mofetil (MMF) or leflunomide (LEF).8
We still have much to learn about the role of these medications. Throughout maintenance therapy, an attempt should be made to taper the prednisone dose as much as possible. The IMPROVE trial suggests that AZT is most effective in maintaining remission (dosed at 2 mg/kg/day), particularly in generalized disease.9 If rituximab were used to achieve disease remission, AZT can be attempted as maintenance, although the MAINRITSAN trial9 found 500 mg of rituximab every six months to be more effective.
The ongoing RITAZAREM trial9 aims to assess the effect of periodic rituximab infusions in addition to maintenance with AZT or methotrexate.
If maintenance therapy fails and remission occurs, induction therapy should be repeated and the subsequent maintenance regimen should be intensified.