HZ cases were identified from the databases of two phase I, nine phase II, six phase III and two long-term extension studies of tofacitinib in RA patients. Crude incidence rates (IRs) of all HZ events (serious and nonserious) per 100 patient-years (with 95% confidence intervals) were calculated for unique patients. Within phase III studies, the researchers described HZ rates according to concomitant csDMARD treatment and baseline corticosteroid use. A multivariable Cox regression model was used to evaluate HZ risk factors across studies.
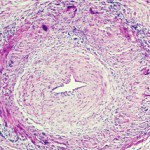
Across all studies (6,192 patients; 16,839 patient-years), HZ was reported in 636 tofacitinib-treated patients (IR 4.0, 95% CI 3.7–4.4). In most cases (93%), HZ was classified as nonserious, and the majority of patients (94%) had involvement of only one dermatome. HZ IRs varied across regions, from 2.4 (95% CI 2.0–2.9) in Eastern Europe to 8.0 (95% CI 6.6–9.6) in Japan and 8.4 (95% CI 6.4–10.9) in Korea. Within phase III studies, HZ IRs varied according to tofacitinib dose, background csDMARD treatment, and baseline use of GCs. The IRs were numerically lowest for monotherapy with tofacitinib 5 mg twice daily without GCs (IR 0.56 [95% CI 0.07–2.01]) and highest for tofacitinib 10 mg twice daily with csDMARDs and GCs (IR 5.44 [95% CI 3.72–7.68]). Age, GC use, tofacitinib dose, and enrollment within Asia were independent risk factors for HZ.
Conclusions
In the first study, patients who began treatment with tofacitinib two to three weeks after receiving LZV had VZV-specific humoral and cell-mediated immune responses to LZV similar to those in placebo-treated patients. Vaccination appeared to be safe in all of the patients except one patient who lacked preexisting VZV immunity.
From a safety standpoint, the single event of disseminated HZ in a patient without prior immunity suggests that patients should be screened for prior immunity (i.e., by eliciting a history of chickenpox or testing with commercially available VZV serologic tests) before administration of this vaccine, or that the time periods between vaccination and initiation of tofacitinib treatment should be longer (e.g., four weeks).
The researchers in the second study found that the risk of HZ is likely to be greater in patients receiving tofacitinib in combination with GCs compared with those receiving monotherapy without GCs. Given that similar efficacy has been observed with tofacitinib in phase III clinical studies regardless of whether it is administered as monotherapy or in combination with csDMARDs and/or GCs, the use of tofacitinib monotherapy without GCs could represent a risk-reduction strategy for physicians and patients with regard to HZ and provide an effective treatment strategy for reduction of the signs and symptoms of RA, provided the patient’s RA remains controlled.