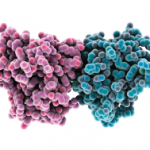
Recent reports have highlighted the importance of the intracellular distribution of HMGB1 in determining its potential biological activity. Inside the cell, in the nucleus, HMGB1 binds to DNA and modulates a variety of processes including the determination of chromosomal architecture and transcriptional regulation. Once translocated from the nucleus and released outside the cell, HMGB1 can function as an inflammatory mediator contributing to many inflammatory processes.6 An important question raised about role of HMGB1 in inflammation relates to whether it can promote inflammation on its own or must operate in tandem with another conventional or nonconventional proinflammatory mediator. Indeed, compelling data indicate that HMGB1 can exert its role as alarmin only when complexed with proinflammatory molecules, endogenous and exogenous substances such as cytokines or TLR ligands.3
In addition to its role in innate immunity, HMGB1 can also modulate events in adaptive immune responses. As shown in a recent study, HMGB1 possesses immunostimulatory properties and can activate dendritic cells (DCs), T-lymphocytes, and B-lymphocytes. Further, data indicate that HMGB1 can mediate the maturation of DCs and their migration of DCs, with DCs both secreting and responding to HMGB1.7 In addition, HMGB1 has an important role in T-cell survival, and enables proliferation and polarization of naive CD4 T-lymphoyctes towards T-helper 1 phenotype (Th-1).8
Other intriguing studies have focused on the effect of HMGB1 on regulatory T cells. Regulatory T cells have important functions in maintaining immunological tolerance, with disturbances in their number or activity predisposing to inflammatory and autoimmune diseases. In animal models, HMGB1 released after injury showed an inhibitory effect on the immunosuppressive function of T-regulatory cells.9 Whether HMGB1 influences the immunosuppressive function of regulatory T cells in the human situation requires further study. Another facet of HMGB1 activity relevant to autoimmunity concerns the ability of this protein to activate autoreactive B-cells and promote their responses to endogenous substances.10 Functions of HMGB1 are summarized in Table 1.
Mode of Action
To function as an alarmin, nuclear HMGB1 must leave the cell to enter the extracellular space where it can interact with various receptors to promote inflammation. Of these receptors, the RAGE was the first identified surface receptor for HMGB1. RAGE is expressed on both immune and nonimmune cells. Ligation of HMGB1 to RAGE activates diverse arrays of intracellular pathway cascades promoting cellular migration. In addition to RAGE, TLR-2 and TLR-4 have been recognized as surface receptor for HMGB1. TLR-2 and TLR-4 are expressed by monoytes, epithelial cells, and renal cells. HMGB1-mediated signaling through TLR-2 and TLR-4 leads to cytokine production. Recently, another TLR member, TLR-9, has been recognized as an intracellular receptor for HMGB1. TLR-9 is expressed by immune cells such as monocytes, B-lymphocytes, and mainly by plasmacytoid dendritic cells (pDCs). TLR-9 recognizes exogenous and endogenous DNA. HMGB1 complexed with DNA enhances cytokine production, mainly IFN-α, in pDCs and induces antibody production from B cells through interacting with TLR-9.2,3
HMGB1 in Diseases with Renal Manifestations
Exciting data indicate that HMGB1 can play an important role in the pathogenesis of chronic inflammatory and autoimmune diseases. Thus, there is evidence that the expression of HMGB1 is increased in the sera of patients in a wide variety of immunologically mediated conditions as well as at sites of local inflammation. In particular, the role of HMGB1 in renal diseases has been explored intensively. In an animal model of adenine-induced nephropathy, granuloma formation was found to be associated with high HMGB1 expression and up-regulation of RAGE and TLR-4 in the kidney. In addition, the presence of HMGB1 worsened the kidney function in rats with granulomatous nephritis.11