Otherwise, vitamin B12 deficiency can cause burning and tingling in the mouth, and vitamin C deficiency can cause mucosal irritation, so it’s worth checking levels. Viral infections, like COVID-19, can trigger a dysautonomia that leads to dry mouth or a dysbiosis with a reset of oral flora that leads to dryness with chronic indolent infection. Certain tongue coatings can suggest dysbiosis, so look at the patient’s tongue and work with their dentist to reset that.
CJ: When it comes to sicca symptoms, the most important don’t miss diagnosis on the differential is hepatitis C viral (HCV) infection. It is more common than SjD and can look identical to it, with fatigue, arthralgia, dryness and gland swelling. Although guidelines recommend that all adults undergo HCV screening at least once in their lifetime, many have not. Another common, and sometimes overlooked, consideration is thyroid disease.
TR: How do you screen patients with SjD for lung involvement?
DD: There’s a great guideline article that recommends high-resolution computed tomography (HRCT) chest without contrast and complete pulmonary function tests (PFTs) in all SjD patients with pulmonary symptoms, and this is how I practice because ILD is so prevalent in SjD.3
CJ: A recent systematic review and meta-analysis showed that the prevalence of ILD in SjD is actually about 20%, which is higher than previously reported.4 The authors note this increased prevalence can be explained by the subset of studies that mandated the use of HRCT in addition to PFTs when screening for ILD. So, you may miss up to half of the ILD in your SjD patients who have cough and/or dyspnea if you use PFTs alone to look for it.
TR: What’s your approach to cancer screening in patients with SjD?
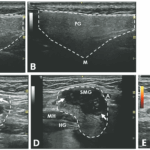
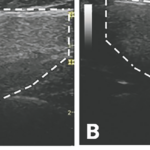
DD: If the patient is seropositive, there is an increased risk of glandular lymphoma. In these patients, I like to check parotid and submandibular ultrasound, as well serum protein electrophoresis with immunofixation (SPEP with IFE), urine protein electrophoresis with immunofixation (UPEP with IFE), and serum free light chains at baseline and at least once a year. I screen more often if they have symptoms like glandular swelling.
TR: Anything to add, Dr. Johr?
CJ: I also ask about salivary gland swelling and have a low threshold to look at the tissue with ultrasound, even if swelling is only intermittent. I ask about B-symptoms (e.g., fever, weight loss, night sweats), but they are only present in about 10% of patients with SjD who have lymphoma. That’s why using the lack of B-symptoms as a way to rule out lymphoma in this population is a mistake.