Managing Ankylosing Spondylitis
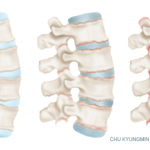
An estimated 2.7 million people in the U.S. have ankylosing spondylitis and related conditions. Ankylosing spondylitis pain begins in the lower back, but it can progress to the hips, shoulders, knees and beyond. Patients may also develop fatigue, fever and trouble sleeping.
Patients with ankylosing spondylitis tend to feel better if they move around, and thus the website suggests that patients maintain an active lifestyle. Specifically, in addition to yoga, the site recommends moderate exercises, such as swimming, biking or walking. The website also notes that an emphasis on good posture may prevent the “bending” effect that is characteristic of ankylosing spondylitis.
Novartis’ Monster Pain in the AS website offers a three-minute quiz to help visitors determine if their symptoms warrant a visit to a rheumatologist.
Many individuals with ankylosing spondylitis also have difficulty sleeping. Stiffness during the night can make it difficult to sleep and can prompt pacing to relieve discomfort. The website thus emphasizes the importance of sleep hygiene and points out that sleep can be helpful in fighting inflammation.
Mr. Reynolds also contributes as an editor to Novartis’ “This AS Life” collection of short films that provide advice to patients living with ankylosing spondylitis.2 One film, for example, addresses the management of pain and flares associated with the condition. In the film, Robert Overbaugh, MD, medical director of pain management services at Cancer Treatment Centers of America in Philadelphia, explains that in the case of his disease, he first experienced iritis. A subsequent neck injury prompted X-rays and an actual diagnosis of ankylosing spondylitis.
In the film, Dr. Overbaugh notes that, for him, although the major symptom of ankylosing spondylitis was fatigue, he also experienced pain. “I’d feel like I was achy. My knees would hurt. My back would hurt,” he explains. The ache could be prompted just from standing. He also emphasizes the stiffness that he feels in the morning and during the night. Dr. Overbaugh finds it helpful to relieve the stiffness with movement, warm showers and consistency with his medication regimen. He also recommends mindfulness, relaxation techniques and biofeedback.
Lastly, Dr. Overbaugh explains when patients with ankylosing spondylitis come to him for pain management, he first tries to determine the underlying cause of a flare. Often, flares are caused by poor sleep, decreased exercise or even an infection. He reminds patients to work to address these underlying triggers of flares and take a holistic approach toward managing the pain of ankylosing spondylitis.