Neuro-rheumatology is a fast-growing field. Better testing and imaging have increased recognition of once-infrequent diagnoses, such as neuro-sarcoidosis and amyloid beta-related angiitis. Concurrently, the rapid expansion of immunotherapy options to treat cancer and their untoward neurological side effects have increased the frequency of referrals to both neurologists and rheumatologists. Identifying and treating neurologic manifestations of systemic diseases can be challenging and requires close collaboration between neurologists and rheumatologists.
Neuro-rheumatology is a fast-growing field. Better testing and imaging have increased recognition of once-infrequent diagnoses, such as neuro-sarcoidosis and amyloid beta-related angiitis. Concurrently, the rapid expansion of immunotherapy options to treat cancer and their untoward neurological side effects have increased the frequency of referrals to both neurologists and rheumatologists. Identifying and treating neurologic manifestations of systemic diseases can be challenging and requires close collaboration between neurologists and rheumatologists.
In Boston, the Brigham and Women’s Hospital neuro-rheumatology clinic was established a few years ago to address this need, and we have gained insight into the challenges associated with caring for these complex patients.
We wish to describe our experience and propose our top five innovations for improved patient care.
1. Encourage interested physicians—neurologists and rheumatologists—to gain expertise in the area of neurorheumatology.
We have an expanding group of clinicians whose training has provided them with enhanced understanding of how systemic and nonsystemic autoimmune diseases intersect with the nervous system. Neurologic manifestations of systemic diseases may occur years before the onset of systemic symptoms.1 Systemic disease can present anywhere in the neurologic system; neurologists with neuro-rheumatology training generally approach patients by localizing their disorder and then narrowing the differential diagnoses using their knowledge of how certain systemic disorders affect the nervous system.2
Because the central nervous system is so complex, it is critical clinicians be qualified to diagnose and manage autoimmune neurologic disorders using all available tools, including magnetic resonance and nuclear medicine imaging, electromyography and appropriate laboratory investigations. By combining the expertise of the neurologist with the rheumatologist, we are better able to manage patients with complicated neurological and systemic features. The shared clinic allows us to break the silos that often isolate one medical specialty from another and eliminate clinical inefficiencies. Many academic neurology programs have instituted fellowship specialty training to enhance the skills of clinicians who wish to pursue their interest in this field.
2. Create a team: the role of the inpatient consult service.
Many patients with neuro-rheumatologic disease present during a hospitalization. These illnesses can range from severe to life threatening. Therefore, we have created a dedicated neuro-inflammatory consult team to assess these patients. This service provides an outstanding opportunity for interested clinicians who wish to gain additional expertise in this field.
Starting our relationship with the patient at the time of their acute illness allows for better short- and long-term management because our team can be involved in developing the appropriate treatment plan, which invariably will require the use of immune-modifying drugs of various complexity.
From a teaching perspective, trainees can better assess the impact their decisions make on the long-term outcome of the patient when they are part of the “team” from the start.
3. Collaboration creates opportunities.
Collaboration with rheumatologists, neurologists and other specialists is critical to the success of our mission. When evaluating patients in the clinic, the physical proximity to others taking care of these patients has been invaluable. For example, we see patients within the clinical area of our rheumatology division, which allows us to see patients together with our rheumatology colleagues. It streamlines the care of patients, greatly improves communication, limits the need for patients to travel and enhances the care we provide.
4. Employ a dedicated administrative assistant.
In our practice, we have found a large range of urgency among referrals and messages. Over the past few years we have acquired the funds to employ an administrative assistant who screens our referrals. She is able to appropriately screen for urgency and contact us if patients need to be seen sooner than time slots are available. Having a dedicated coordinator allows us to exclude patients who may not be appropriate for the clinic. This ultimately improves our accessibility and allows the best utilization of resources.
5. Incorporate a physician assistant.
As with many other neurology specialties, wait times to be seen in our clinics have increased with expected increasing demand.3 It has been well documented that integration of physician assistants into the care of patients receiving chemotherapy (like many of our patients do) and for neurology patients reduces wait times.4,5 The addition of an advanced practice provider to our group has allowed better access to our clinics and safer patient monitoring. We utilize our physician assistant to arrange rapid follow-up on inpatients. We also have regularly scheduled visits in between visits for drug and disease monitoring.
Through these clinic advances, we have found increased patient and physician satisfaction. Our collaborations within divisions, providers and administrators have allowed us to deliver more holistic care. We anticipate future evolution in our clinic to include the collaborative development of guidelines, collection of biomaterials and further expansion into clinical trials.
The Clinic in Action
A 58-year-old man with a history of heart failure, chronic kidney disease, diabetes and rheumatoid arthritis being treated with etanercept presented to his rheumatologist for routine care and was noted to have significant difficulty walking.
The patient reported he developed COVID-19 and recovered well. One month later, he developed sharp burning pain, numbness and weakness in both of his arms and legs. His rheumatologist was concerned and sent an initial request for an evaluation of polyneuropathy and messaged the neuro-rheumatologist for urgent referral.
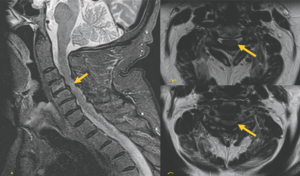
FIGURE 1 (Click to enlarge.)
Left: T2 STIR Sagittal MRI shows multi-degenerative disc disease with severe stenosis and abnormal cord signal at C4-C5.
Top right: Axial T2 at the C3-C4 level shows posterior disc osteophyte complex effacing the majority of the CSF space.
Bottom right: Axial T2 at the C4-C5 Posterior disc osteophyte complex, which effaces the ventral CSF space that contacts and deforms the spinal cord and ligamentum flavum buckling.
Due to the embedded nature of the clinic and rapidly worsening walking, the patient was added to the neurologist’s schedule two weeks later. At his neurology visit, additional screening revealed he had severe neck pain and intermittent bowel and bladder incontinence. His exam was notable for reduced strength in both arms, distally more than proximally; reduced strength at both hips; brisk reflexes, with the exception of the ankles, which were reduced; and a sensory exam notable for reduced sensation at the great toes and hands.
Based on the exam, with sensory loss in a non-dermatomal or length-dependent distribution and additional neck pain and bowel and bladder involvement, a myelopathy superimposed on a peripheral neuropathy was suspected. The patient was sent for urgent spinal imaging, which showed severe spinal stenosis with abnormal cord signal (see Figure 1).
He was referred urgently to neurosurgery and underwent C2-5 laminectomy and medical fasciotomy. At follow-up one month later he had recovered his ability to perform activities of daily living including buttoning his shirt and using his computer. He also regained strength in his legs and was able to use a walker.
 Kristin Galetta, MD, is an instructor of neurology in the Department of Neurology, Brigham and Women’s Hospital and Harvard Medical School, Boston.
Kristin Galetta, MD, is an instructor of neurology in the Department of Neurology, Brigham and Women’s Hospital and Harvard Medical School, Boston.
 Shamik Bhattacharyya, MD, is an assistant professor in the Department of Neurology, Harvard Medical School, Boston.
Shamik Bhattacharyya, MD, is an assistant professor in the Department of Neurology, Harvard Medical School, Boston.

Dr. Helfgott
Simon M. Helfgott, MD, is an associate professor of medicine in the Division of Rheumatology, Immunology and Allergy at Harvard Medical School, Boston, and a previous physician editor of The Rheumatologist.
Disclosures
Dr. Galetta has received personal compensation for consulting from Glaxo Smith Kline.
Dr. Bhattacharyya has received consulting fees from Alexion Pharmaceuticals, Teladoc Health, and Glaxo Smith Kline unrelated to this project; research support from the National Institutes of Health and Alexion Pharmaceuticals; and publishing honorarium from American Academy of Neurology and UpToDate.
Dr. Helfgott has received royalty payments from UpToDate unrelated to this project.
References
- McManus EJ, Phillips MC, Schepel J, et al. Neurological manifestations in rheumatological disease, a case series. Neuroimmunology Reports. 2022 Jan 1;2:100075.
- Goglin S, Cho TA. Clinical approach to neurorheumatology. J Neurol Sci. 2021 Dec 15;431:120048.
- Freeman WD, Vatz KA, Griggs RC, et al. The Workforce Task Force report: clinical implications for neurology. Neurology. 2013 Jul 30;81(5):479–486.
- Hardeman P, Hough R. Integration of advanced practice clinicians in neurology practices. JAMA Neurol. 2017 Aug 1;74(8):894–895.
- Glotzbecker BE, Yolin-Raley DS, DeAngelo DJ, et al. Impact of physician assistants on the outcomes of patients with acute myelogenous leukemia receiving chemotherapy in an academic medical center. J Oncol Pract. 2013 Sep;9(5):e228–233.