Sessions at the 2019 ACR/ARP Annual Meeting, Nov. 8–13 in Atlanta, will include less didactic learning formats—fewer lectures from lecterns and more conversation-style talks. This year’s Meet the Professor Workshops and courses are no exception. Their topics are cutting edge, with seating arrangements that will spark dialogue and ample time for the experts in their fields to answer questions.
“These sessions purposely have limited enrollment to control how many learners are in the room, so each person can get what they need,” says Rebecca Manno, MD, MHS, assistant professor of medicine at Johns Hopkins University, Baltimore, and assistant director of the Johns Hopkins Vasculitis Center. Dr. Manno also chaired the subcommittee that planned the sessions.
These sessions require an additional registration fee. Meet the Professor courses are $50 for members and $75 for non-members. Workshops are $100 for members and $150 for non-members.
Workshops feature practical, hands-on training in procedural skills using specialized equipment, or animal and silicon models. Meet the Professor sessions are designed for deep-dive discussions with experts.
“We encourage attendees to bring their cases or images. They will walk away from these sessions with the solutions to their questions,” says Dr. Manno.
The Expert Viewpoints
Rheumatologists who see an increase in patients referred with immunotherapy-associated arthritis symptoms will benefit by attending Checkpoint Inhibitors, a Meet the Professor course.
“Checkpoint inhibitors are being used to treat an ever-expanding list of cancers. Whether you work in an academic center or in private practice, you are likely to see patients experience immune-related adverse events from these powerful medications, including checkpoint inhibitor-associated arthritis,” says the speaker, Anne R. Bass, MD, rheumatology fellowship program director at the Hospital for Special Surgery, New York.
Patients’ symptoms may mimic rheumatoid arthritis and respond to steroids and tumor necrosis factor inhibitors. “However,” she says, “treatment has to balance arthritis control with maintaining the checkpoint inhibitor’s anti-cancer effect. Identifying the safest disease-modifying anti-rheumatic drugs and biologics to use in this setting is a research priority.”
Another Meet the Professor session, Imaging of Large-Vessel Vasculitis, will be led by Peter Grayson, MD, MSc, head of the Vasculitis Translational Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases. He will discuss how to image these vessels and interpret the results.
“Dr. Grayson will share his own stockpile of images. He is a true leader of this field,” says Dr. Manno. “As rheumatologists, we’re so limited in diagnostic tools for large-vessel vasculitis, and imaging is it, because we cannot biopsy the aorta. This discussion will explore the foundation of how we manage these diseases.”
Other Meet the Professor sessions at the 2019 Annual Meeting will include:
- Musculoskeletal Radiology: Pearls for the Rheumatologist—speaker John A. Carrino, MD, MPH, vice chair of radiology at the Hospital for Special Surgery, will discuss a wide array of imaging options for diagnosis of arthropathies, including uncommon or rare diseases, and how to interpret findings that may overlap with multiple diagnoses, as well as how rheumatologists may work with radiologists to manage these cases;
- CNS Vasculitis and Its Impostors—speaker Rula Hajj-Ali, MD, staff physician at Cleveland Clinic’s Center for Vasculitis Care and Research, will conduct a case-based, interactive discussion about the diagnosis and optimal management of primary and secondary central nervous system vasculitis and address how to distinguish it from mimics; and
- Management of Rheumatic Disease Patients Undergoing Arthroplasty—speaker Susan M. Goodman, MD, a rheumatologist at the Hospital for Special Surgery, will discuss evidence on perioperative complications, including venous thromboembolism, infections and periprosthetic fracture, for patients with various rheumatic diseases who have total hip or knee replacement. The talk will clarify the rationale behind management options and make it easier to discuss treatment choices with patients.
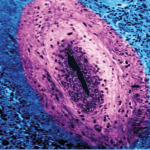
Workshops: Refine Skills
One of the new Workshops this year is Hands-On Approach to Perform Salivary Gland (Lip) Biopsy, with instructors Robert W. Ike, MD, associate professor of medicine at the University of Michigan, Ann Arbor, and Sara S. McCoy, MD, assistant professor of medicine, University of Wisconsin School of Medicine and Public Health, Madison. They will review the indications, risks and histopathologic interpretation of minor salivary glands, then devote most of the session to practicing biopsy techniques.
Rheumatologists may not be comfortable with small procedures, such as mucosal incisions and simple sutures, says Dr. McCoy.
“We will recreate an environment in which rheumatologists can practice their technique on animal-model simulations. The end goal of this workshop is to make rheumatologists comfortable with the utilization of the minor salivary gland biopsy in their practice,” she says. “The minor salivary gland biopsy is a major part of diagnostic criteria for Sjögren’s syndrome and can serve clinically to differentiate seronegative Sjögren’s syndrome patients from patients with xerostomia and no systemic autoimmune disease.”
Minor salivary gland biopsy may be used to evaluate patients for Sjögren’s mimics, such as sarcoidosis and lymphoma, and for prognostication regarding risk of lymphoma in Sjögren’s syndrome. “Despite the clinical relevance of the minor salivary gland biopsy, the process of referring patients outside of rheumatology for biopsy is time-intensive and costly to patients,” says Dr. McCoy. “By providing the biopsy as part of standard rheumatology office practice, we can improve the cost and convenience of this procedure for our patients.”
Other Workshops at the 2019 Annual Meeting will include:
- Ultrasound of Psoriatic Dactylitis and Enthesitis—speakers George Bruyn, MD, PhD, professor of rheumatology at Reumakliniek Flevoland, Lelystad, The Netherlands, and Natalie Faith, MD, RhMSUS, RMSK, a rheumatologist at Florida Medical Clinic, Land O’Lakes, will review the anatomy and important ultrasound features of psoriatic arthritis and how to assess multiple entheseal sites, as well as the extensor and flexor tendons of the fingers and toes;
- Advanced Musculoskeletal Physical Exam Skills: Diagnosis of Common and Uncommon Shoulder and Knee Disorders—speaker Jean Gillies, MD, a rheumatologist at the University of British Columbia, Vancouver, Canada, will provide training in basic and advanced exam techniques, and how to interpret the findings to make accurate diagnoses of soft-tissue shoulder and knee disorders, which often lack gold standard screening tests. She will demonstrate how to use a goniometer to measure joint range of motion and how to evaluate patients for office-based, palpation-guided periarticular injections to reduce symptoms and improve joint function; and
- Synovial Fluid Analysis and Crystal Identification—speakers Brian Mandell, MD, PhD, and Mathilde Pioro, MD, both rheumatologists at the Cleveland Clinic, will address synovial fluid analysis. Anyone who lacks confidence in performing synovial fluid analysis, which is used to definitively diagnose gout and pseudogout, will benefit from hands-on training in this important skill, says Dr. Manno. This wet-lab workshop includes polarized microscopes for each participant.
Susan Bernstein is a freelance journalist based in Atlanta.
Join Us at the Annual Meeting
The 2019 ACR/ARP Annual Meeting, Nov. 8–13, in Atlanta is your gateway to global rheumatology education. View the Online Program to find out more about the opportunities for professional development and networking, and obtain firsthand access to the latest rheumatology research and clinical applications. Register now, and don’t miss out.