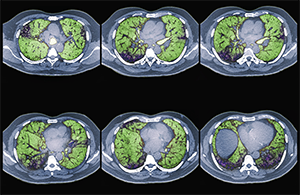
Colored CT scans of axial sections through the chest of a 68-year-old patient with ILD.
Zephyr/ScienceSource.com
SAN FRANCISCO—Interstitial lung disease (ILD) represents a heterogeneous group of disorders characterized by inflammation or fibrosis of the lungs. The disorders are also associated with a spectrum of connective tissue diseases (CTDs).
ILD is a common manifestation of CTDs, such as scleroderma, poly-/dermatomyositis and rheumatoid arthritis—and is a leading cause of morbidity and mortality in these conditions, said Aryeh Fischer, MD, associate professor of medicine in the Divisions of Rheumatology and Pulmonary Sciences at the University of Colorado, during a full-day conference devoted to ILD sponsored by the University of California-San Francisco on Nov. 5, 2016.
“It is important to consider the intersection of CTD and ILD as a spectrum of diseases. Inherently, we believe these conditions each likely behave differently and may respond to treatment differently,” said Dr. Fischer.
Aryeh Fischer, MD
The recognition that an ILD is associated with CTD affects prognostication and management, and provides a clinical context for understanding extrathoracic manifestations of disease. A diagnosis of a CTD can also address some of the frustrations ILD patients feel about being labeled “idiopathic.” Roughly 30% of patients presenting to an ILD center presumed to have an idiopathic ILD will have an underlying CTD as the cause of their ILD, Dr. Fischer noted.
Many patients with ILD have subtle features suggestive of an autoimmune etiology, but current strategies and even terminology for identifying and classifying these patients can be controversial and inadequate, he said. What about ILD patients who present without any extra-thoracic symptoms? According to traditional classifications, they are not considered to be “rheumatologic” patients, but Dr. Fischer led a joint European Respiratory Society and American Thoracic Society task force that recently proposed a new classification category, “interstitial pneumonia with autoimmune features” (IPAF).1
The multidisciplinary approach is the gold standard for diagnosing and treating these conditions, speakers noted, and the conference illustrated that approach with a panel discussion comprising a pulmonologist, radiologist, pathologist and rheumatologist. Dr. Fischer, the rheumatologist, said he became professionally intrigued by the intersection between the two disease categories. “I have been fortunate to find a home at a respiratory center at the University of Colorado as part of a multidisciplinary ILD program.”
To Biopsy or Not
How do you diagnose these conditions? Be a really good clinician, speakers noted. But expect it to be a challenge. “Before we conclude that an ILD is CTD related, we need to consider alternate etiologies. Does the ILD pattern fit? What else could have caused the lung disorder?” Dr. Fischer posed.


