An in-depth review of Janus kinase inhibitors, their risks & more
An in-depth review of Janus kinase inhibitors, their risks & more
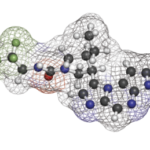
BARCELONA—Of the many advanced therapies available to rheumatologists for the treatment of their patients, Janus kinase (JAK) inhibitors are among the most interesting because they are administered orally and have a wide range of potential uses. However, they have also been associated with an increased risk of specific adverse events.
In the EULAR 2025 session, JAK It Out: New Perspectives on JAK Inhibitors, several speakers provided insights into these medications.
The Basics
The JAK-signal transducer and activator of transcription (STAT) pathway is central to immune dysregulation in many autoimmune diseases due to its role in transducing signals from an array of cytokines that regulate both innate and adaptive immunity.
In rheumatoid arthritis (RA), pro-inflammatory cytokines, such as interleukin (IL) 6, interferon-γ and GM-CSF, signal through JAKs, leading to STAT activation and transcription of genes that drive synovial inflammation, pannus formation and joint destruction. In other immune-mediated inflammatory diseases (IMIDs), such as systemic lupus erythematosus (SLE) and giant cell arteritis (GCA), aberrant activation of the JAK-STAT pathway leads to excessive production of pro-inflammatory cytokines, loss of immune tolerance and propagation of autoreactive lymphocytes.1
Conditions Treated with JAK Inhibitors
With this basis in mind, Andreas Kerschbaumer, MD, PhD, postdoctoral fellow, Division of Immunology and Rheumatology, Stanford University School of Medicine, Palo Alto, Calif., summarized the use of JAK inhibitors in a host of IMIDs.
JAK inhibitors—including tofacitinib, baricitinib, upadacitinib, filgotinib and others—have demonstrated significant efficacy in patients with RA, with multiple phase 3 clinical trials and meta-analyses showing superiority over placebo and, in some studies, over methotrexate and tumor necrosis factor (TNF) α inhibitors. In psoriatic arthritis, axial spondyloarthritis and inflammatory bowel disease, JAK inhibition has also demonstrated efficacy, with clinical trial data supporting their use for improving both the articular and extra-articular disease manifestations of these conditions.2
Dr. Kerschbaumer noted a recent phase 3 study on the use of upadacitinib in GCA as particularly interesting. In this randomized, placebo-controlled trial, patients with new-onset or relapsing GCA were assigned to receive either 15 mg or 7.5 mg of upadacitinib daily with a 26-week glucocorticoid taper or placebo with a 52-week glucocorticoid taper. The study’s primary end point was sustained remission at week 52.
At week 52, the 15 mg dose of upadacitinib given daily demonstrated superior efficacy compared with placebo, with about 46% of patients achieving the end point in the upadacitinib arm compared to 29% in the placebo arm. The 7.5 mg dose of upadacitinib given daily did not demonstrate superiority over placebo.3 Based largely on the strength of this study, the U.S. Food & Drug Administration approved the dose of 15 mg of daily upadacitinib for the treatment of adults with GCA in April.4