Clinical Pearls in TMJ Arthritis
The TMJ, one of the most frequently used joints in the body, continues to mature during a person’s twenties. “Even subtle dysfunction can cause significant daily pain and functional issues,” Dr. Gakhal said.
The scientific literature reports a wide range in incidence of TMJ involvement in patients with JIA likely due to different diagnostic methods and patient populations, but it may be quite frequent. Relatedly, TMJ involvement is often difficult to diagnose early because inflammation may be initially asymptomatic or subtle in presentation, and structural damage may already be present at the time of diagnosis.
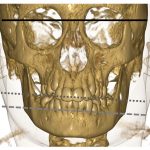
Untreated TMJ arthritis can cause quite significant complications, impairing such tasks as eating and speaking and causing other problems, such as receding jaw or jaw underdevelopment, teeth misalignment, facial asymmetry and sleep apnea.
“Decreased maximal jaw opening is the sign most indicative of TMJ involvement,” Dr. Gakhal said. A simple way to assess this symptom is by seeing the number of finger breaths the patient can fit in their mouth. Less than three often indicates a problem. More formally, one can measure the distance between the patients upper and lower incisors when they open their jaw as wide as possible. This measurement should be at least 40 mm or more.8
Other joint findings may include deviation of the mandible, tenderness or crepitus while opening the jaw or tenderness of the masticatory muscles. It is important to note the TMJ is also prone to mechanical issues unrelated to JIA that may appear on physical exams or imaging.
Dr. Gakhal explained that X-ray and ultrasound are of limited utility, and magnetic resonance imaging (MRI) is the diagnostic gold standard. However, she emphasized that it must be performed with gadolinium contrast, using a specific MRI protocol for inflammatory disease, as opposed to the type of scan that may be used for head and neck cancer.
These images should be interpreted by a radiologist with expertise in musculoskeletal inflammatory disease and involvement of the TMJ. An expert can help distinguish the bone marrow edema and contrast enhancement consistent with synovitis from active JIA from reactive synovitis from prior damage or reactive synovitis from unrelated mechanical issues.
For treatment, a specialized physiotherapist with expertise in TMJ involvement can be very helpful. Dr. Gakhal noted that oral nonsteroidal anti-inflammatory drugs have limited value. Conventional DMARDs, such as methotrexate, may be needed, escalating to biologic DMARDs, such as TNF-inhibitors or tocilizumab, if indicated.9