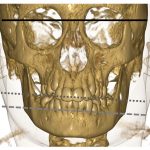
“Use cortisone injections sparingly and with caution,” Dr. Gakhal said, “because they can affect the mandibular growth in an immature skeleton.”
 Ruth Jessen Hickman, MD, a graduate of the Indiana University School of Medicine, is a medical and science writer in Bloomington, Ind.
Ruth Jessen Hickman, MD, a graduate of the Indiana University School of Medicine, is a medical and science writer in Bloomington, Ind.
ad goes here:advert-1
ADVERTISEMENT
SCROLL TO CONTINUE
References
- Sandborg CI, Schulert GS, Kimura Y. Juvenile idiopathic arthritis. N Engl J Med. 2025 Jul 10;393(2):162–174.
- Angeles-Han ST, Ringold S, Beukelman T, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the screening, monitoring, and treatment of juvenile idiopathic arthritis-associated uveitis. Arthritis Care Res (Hoboken). 2019 Jun;71(6):703–716.
- Berard R, Ng HY, Human A, et al. Canadian Rheumatology Association recommendations for the screening, monitoring, and treatment of juvenile idiopathic arthritis-associated uveitis. J Rheumatol. 2023 Mar;50(3):390–399.
- Foeldvari I, Bohn M, Petrushkin H, et al. A practical approach to uveitis screening in children with juvenile idiopathic arthritis. Br J Ophthalmol. 2025 Feb 24;109(3):372–376.
- Rypdal V, Glerup M, Songstad NT, et al. Uveitis in juvenile idiopathic arthritis: 18-year outcome in the population-based Nordic cohort study. Ophthalmology. 2021 Apr;128(4):598–608.
- Marino A, Cicinelli MV, Miserocchi E, et al. Recurrence risk in pediatric noninfectious uveitis during adalimumab tapering: An international multicenter retrospective study. Arthritis Rheumatol. 2025 Sep;77(9):1254–1262.
- Acharya NR, Ramanan AV, Coyne Abet al. Stopping of adalimumab in juvenile idiopathic arthritis-associated uveitis (ADJUST): A multicentre, double-masked, randomised controlled trial. Lancet. 2025 Jan 25;405(10475):303–313.
- de Sonnaville WFC, Speksnijder CM, et al. Clinically established temporomandibular involvement in adults with juvenile idiopathic arthritis. J Rheumatol. 2023 Nov;50(11):1462–1470.
- Onel KB, Horton DB, Lovell DJ, et al. 2021 American College of Rheumatology guideline for the treatment of juvenile idiopathic arthritis: Therapeutic approaches for oligoarthritis, temporomandibular joint arthritis, and systemic juvenile idiopathic arthritis. Arthritis Rheumatol. 2022 Apr;74(4):553–569.