Kateryna Kon / shutterstock.com
CHICAGO—At the 2018 ACR/ARHP Annual Meeting, Allen C. Steere, MD, delivered the Rheumatology Research Foundation Memorial Lecture honoring the late Charles M. Plotz, MD: Linking Gut Microbial Immunity with Autoimmunity in Joints in Patients with Rheumatoid Arthritis. Dr. Steere is professor of medicine at Harvard Medical School, Boston, and director of translational research in rheumatology at Massachusetts General Hospital. His ongoing research focuses on the possible role of infectious agents in the microbiome, particularly Prevatella copri, in the initiation and perpetuation of pathogenic immune responses in rheumatoid arthritis (RA).
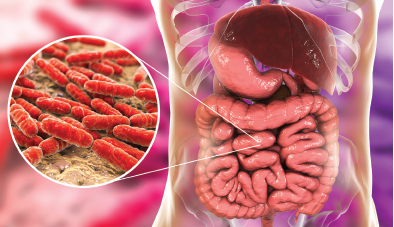
Bacterial Colonies in the Gut
Rheumatologists have made great progress in understanding RA’s genetic risk factors, but are only now identifying its environmental factors, said Dr. Steere. His lecture focused on the gut as a potential site of immune stimulation.
“Most of the microbiota is in the gut—more than 1,000 bacterial species and over 1 trillion bacterial cells,” he said. Dysbiosis, or a disruption of the normal balance in the microbial commensal ecosystem, with narrowing diversity, may result in disease.2 Gut dysbiosis has been demonstrated in rheumatic diseases like RA, ankylosing spondylitis, psoriatic arthritis and reactive arthritis. Implicated organisms in these diseases vary, but one common feature is reduction in diversity, allowing expansion of certain species.
“The hypothesis,” said Dr. Steere, “is that with narrowed commensal diversity, certain organisms are able to expand, attach to and invade the gut mucosa, where they promote an exaggerated immune response, activating systemic inflammation in a way that contributes to joint disease.”3
A 2010 study using K/BxN TCR transgenic mice showed the importance of segmented filamentous bacteria (SFB) and Th17 responses in arthritis development.4 These mice are engineered to develop arthritis as a response to glucose-6-phosphate isomerase (GPI). The study showed the mice did not develop arthritis in a germ-free environment, “but the introduction of SFB in germ-free mice was sufficient to reinstate Th17 cells, leading to the production of autoantibodies and arthritis, and neutralization of IL-17 prevented arthritis,” he said.
Humans do not have SFB. Can other organisms in humans’ microbiota induce this type of response? The answer is yes, said Dr. Steere. In a 2017 study, IgA-coated E. coli bacteria promoted Th17-dependent inflammation in patients with Crohn’s disease-related spondyloarthritis (SpA).5 They determined the identity of bacterial strains by 16S rDNA sequencing, and showed that only one bacterial taxon, E. coli Shigella, was significantly different between the two patient groups. E. coli were more often coated with IgA in patients with Crohn’s SpA than in those with just Crohn’s disease.
“What’s more, the height of the coating index to E. coli correlated with the BASDAI score in terms of the arthritis being more severe,” he said. Fifteen E. coli isolates from three patients were an invasive-adherent strain of the bacterium. Typically, commensal E. coli strains are neither adherent nor invasive. “Attachment and invasion of the organism to intestinal mucosa explains why the organism would activate Th17 responses.”
These authors conducted a study of KBxN mice and found that anti-GPI antibody titers were similar when the mice were inoculated with SFB or with the invasive-adherent E. coli strain isolated from the patients in the study. “This mouse is engineered to have autoantibody responses to GPI, but an organism implicated in human Crohn’s SpA, an invasive-adherent E. coli strain, was sufficient to cause Th17 responses and autoimmune arthritis in this model system,” Dr. Steere said.


