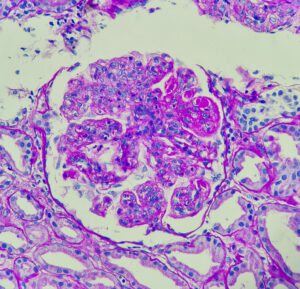
Lupus nephritis, showing wire loop and hyaline thrombi, PAS stain, magnification 400x, photo under microscope; ADOBE STOCK | Chutima
WASHINGTON, D.C.—At a Nov. 18 session of ACR Convergence 2024, speakers shared key elements of the upcoming guideline on the screening, treatment and overall management of lupus nephritis in children and adults. This guideline attempts to balance the risks of medication side effects with the important goal of preserving kidney function.
This is the ACR’s first lupus guideline since 2012. At that time, recommendations were made for induction therapy with high-dose glucocorticoids plus immunosuppressant medications, such as mycophenolate mofetil (MMF) or cyclophosphamide, with MMF often used as a maintenance therapy.1
Since then, more information has become available regarding additional effective agents, and the U.S. Food & Drug Administration has approved both belimumab (a B cell inhibitor) and voclosporin (a calcineurin inhibitor) for the treatment of lupus nephritis. Although rates have been declining, up to 20% of lupus nephritis patients have faced end-stage renal disease within the first decade of diagnosis. New therapies and therapeutic strategies may provide better results.2
This guideline follows the established ACR guideline development format. It is based on a systematic litereature review with input from a patient panel, adult and pediatric rheumatologists and nephrologists, and a rheumatology physician assistant.
Screening & Biopsy
In patients with lupus but without known kidney disease, screening for proteinuria every six to 12 months is a strong recommendation. It’s also strongly recommended that patients with systemic lupus erythematosus (SLE) receive a proteinuria screening if they experience a disease flare in another organ system.
The guideline also emphasizes the importance of prompt kidney biopsy if lupus nephritis is suspected, which can help facilitate timely treatment. Biopsy in the case of proteinuria greater than 0.5g/g or other signs of unexplained impaired kidney function are conditional recommendations.
Additionally, a repeat kidney biopsy is conditionally recommended in patients previously in lupus nephritis remission who present with suspected flare. Kidney biopsy is also recommended for patients who’ve had appropriate treatment but ongoing signs of disease, such as ongoing proteinuria, hematuria or decreased kidney function.

Dr. Sammaritano
Lisa R. Sammaritano, MD, a professor of clinical medicine at Weill Cornell Medicine and Hospital for Special Surgery, New York, and the lead author on the guideline, noted that clinicians should not wait for biopsy results to give glucocorticoids if lupus nephritis is suspected.
Triple Therapy Treatment
A key element of the guideline is its emphasis on triple therapy for new onset or flaring lupus nephritis. In this context, triple therapy consists of glucocorticoids (i.e., high-dose, pulse intravenous [IV] glucocorticoids followed by an oral taper) given with two additional immunosuppressive therapies.
Dr. Sammaritano explained the preference for triple over dual therapy. She noted that the best current randomized controlled trials on the topic, such as the BLISS-LN study with belimumab and the AURORA trial with voclosporin, show improved outcomes with the addition of another immunosuppressant without greater adverse events.3,4
“Nephron loss continues throughout a person’s lifetime, and every episode of lupus nephritis changes the course of that decline for the worse,” Dr. Sammaritano said. “So we feel we can’t wait for nephron loss to implement what has been shown to be the most efficacious therapy.”
Typically, these additional immunosuppressives should be:
- MMF—or an analogue, such as mycophenolic acid—plus belimumab;
- MMF with a calcineurin inhibitor (e.g., voclosporin, tacrolimus and cyclosporine); or
- Low-dose cyclophosphamide—as established in the EuroLupus Nephritis Trial—plus belimumab, with MMF switched in after the initial course of cyclophosphamide is complete.5
Also, MMF-based regimens are conditionally recommended over cyclophosphamide-based regimens in patients with class III or class IV lupus nephritis, which Dr. Sammaritano explained is largely due to safety concerns. For patients with extra-renal disease, triple therapy containing belimumab is the conditional recommendation. If cyclophosphamide is used, it should be the lower dose protocol.
Another specific, conditional recommendation is for MMF plus a calcineurin inhibitor plus corticosteroids to be used if proteinuria is greater than 3g/g creatinine in class III, class IV nephritis or if over 1g/g creatinine in class V (membranous) nephritis, which is less common. Dr. Sammaritano explained that was due to the stabilizing effects of calcineurin inhibitors on the podocyte cytoskeleton.
“We do not specifically recommend cyclophosphamide with a calcineurin inhibitor as one of our options because this combination has not been studied in randomized controlled trials,” said Dr. Sammaritano. “But this does not mean that this combination cannot be used when indicated.”
Corticosteroids
In line with other recent ACR guidelines, this guideline attempts to limit doses of glucocorticoids and their consequent toxicities. Therefore, pulse IV glucocorticoids followed by low to moderate doses of oral glucocorticoids (i.e., 0.5 mg/kg/day with a max dose of 40 mg/day, tapering to a target dose of less than 5 mg/day by six months) are conditionally recommended.
Dr. Sammaritano described a recent meta-analysis that found that pulse glucocorticoids followed by a lower dose of oral glucocorticoids maximized complete renal response while minimizing toxicity.6 Moreover, she noted that patient panel participants strongly desired lower glucocorticoid doses if possible.
Treatment Duration & Monitoring
Lupus nephritis requires extended treatment to decrease the risk of flares. Thus, it is conditionally recommended that patients who have achieved a complete renal response extend their treatment period to at least three to five years, whether they were receiving triple or dual therapy.
“Repeat kidney biopsy shows that immunologic activity persists for several years and withdrawal of immunosuppression predisposes patients to lupus flare,” Dr. Sammaritano said.
The guideline includes two strong recommendations for monitoring. For patients whose renal disease has not completely responded to therapy, proteinuria should be quantified at least every three months. In patients who have shown a sustained and complete response, proteinuria should still be monitored, but this timeframe can be stretched to every three to six months.
Implementation
The guideline also contains additional recommendations and good practice statements on other aspects of care, including adjunctive treatments, refractory disease and renal replacement therapy. A guideline summary is now available that includes 41 recommendations and good practice statements. The full guideline manuscript is expected to be available in late spring or early summer 2025.
Dr. Sammaritano recognized that some patients face barriers in access to newer medications.
“We are mindful of [these barriers], and available traditional therapies should absolutely be used if recommended medications are not available,” she said. “But we do hope to encourage rheumatologists to be somewhat more aggressive in their treatment with the hope that, overall, this new generation of patients who are battling lupus nephritis will have better outcomes than we have seen in the past.”
For more information, watch this video from Dr. Sammaritano.
Ruth Jessen Hickman, MD, a graduate of the Indiana University School of Medicine, is a medical and science writer in Bloomington, Ind.
References
- Hahn BH, McMahon MA, Wilkinson A, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res (Hoboken). 2012 Jun;64(6):797–808.
- Parodis I, Tamirou F, Houssiau FA. Prediction of prognosis and renal outcome in lupus nephritis. Lupus Sci Med. 2020 Feb 18;7(1):e000389.
- Furie R, Rovin BH, Houssiau F, et al. Two-year, randomized, controlled trial of belimumab in lupus nephritis. N Engl J Med. 2020 Sep 17;383(12):1117–1128.
- Rovin BH, Teng YKO, Ginzler EM, et al. Efficacy and safety of voclosporin versus placebo for lupus nephritis (AURORA 1): A double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2021 May 29;397(10289):2070–2080.
- Houssiau FA, Vasconcelos C, D’Cruz D, et al. Immunosuppressive therapy in lupus nephritis: The Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum. 2002 Aug;46(8):2121–2131. doi:10.1002/art.10461
- Figueroa-Parra G, Cuéllar-Gutiérrez MC, González-Treviño M, et al. Impact of glucocorticoid dose on complete response, serious infections, and mortality during the initial therapy of lupus nephritis: A systematic review and meta-analysis of the control arms of randomized controlled trials. Arthritis Rheumatol. 2024 Sep;76(9):1408–1418.