(click for larger image)
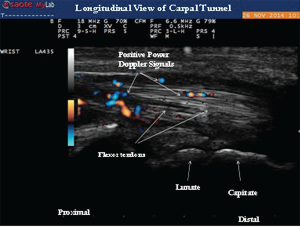
Image 4: Longitudinal view of the carpal tunnel demonstrating the positive power Doppler signals between the flexor tendons.
In early RA, acute-phase reactants, serologies and plain radiographs can be normal, making the history and physical examination of primary importance to the diagnosis. MSK ultrasound can enhance diagnostic certainty for the diagnosis of RA because subtle clinical exam signs of synovitis or tenosynovitis can be quite obvious on ultrasound examination. In addition, MSK ultrasound can provide reliable imaging findings for the presence of crystalline arthropathies, which can be helpful in identifying the crystalline mimics of RA.
EULAR recommendations for use of imaging of joints in clinical management of patients with RA support the use of ultrasound at various disease stages. Ultrasound can be used to diagnose RA when there is diagnostic uncertainty, and this imaging modality can accurately detect joint inflammation (superior to clinical examination). Ultrasound should be considered in patients with early RA if conventional radiography is normal and exam findings are questionable for active tenosynovitis or synovitis. It’s useful to monitor disease activity and progression, to predict further joint damage as a prognostic indicator, and to predict treatment response. Moreover, ultrasound can detect inflammation during clinical remission and predict subsequent joint damage by assessing persistent inflammation as defined by positive power Doppler activity.4 In addition, as in our patient, ultrasound imaging can provide objective evidence of active synovitis, which can be of value when educating patients on the importance of initiating DMARD therapy.
(click for larger image)
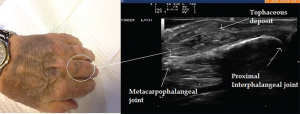
Image 5: Ultrasound image of inhomogeneous hyperechoic signals in the soft tissue appearance. The area was suggestive of tophi and aspirated under ultrasound guidance with confirmation.
Case 2
A 73-year-old male with a past medical history significant for renal transplant secondary to polycystic kidney disease presented to the rheumatology office with complaints of soreness and swelling in his left third proximal interphalangeal joint (PIP) for a duration of two months. His immunosuppressive regimen included tacrolimus and prednisone 5 mg daily. The patient also had pain and swelling associated with stiffness in both ankles.
His chronic joint complaints were suggestive of either RA or a microcrystalline process. On examination he had soft tissue swelling of the third PIP joint with adjacent fullness of the proximal phalanx. No visible cutaneous tophi were appreciated on exam.
The EULAR recommendations for CPP deposition suggest that ultrasound is more sensitive & specific than X-rays for peripheral joints.
Ultrasound imaging of the third PIP revealed peri-articular swelling with hyperechoic signals in a focal aggregate associated with surrounding positive power Doppler signals (see Images 5 & 6). The area was aspirated under ultrasound guidance revealing tophaceous material (see Image 5 confirmed with a polarizing microscope examination. The patient was maintained on low-dose steroids and then transitioned to the uricosuric agent febuxostat with gradual improvement of his symptoms. His uric acid level on his initial visit was 8.6 mg/dL, which improved to 4.5 mg/dL. Of note, the patient was not on cyclosporine, which increases the propensity to development of gout in transplant patients. He was on low-dose prednisone for his renal transplant, which may have masked the typical presentation of gout. Of interest, the ultrasound of the intermittently symptomatic right ankle demonstrated double contour sign of the tibiotalar joint (see Image 7).