(click for larger image)
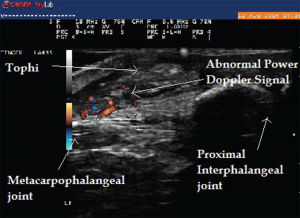
Image 6: Abnormal power Doppler signals suggestive of inflammation and high vascularity in the same patient.
Several findings on the musculoskeletal ultrasound are characteristic of gout. Hyperechoic spots less than 1 mm in size within anechoic synovial fluid can result in a “snowstorm appearance,” with movement of these deposits within the synovial fluid. Tophi deposits have a varied appearance and can be seen as a circumscribed, inhomogeneous, hyperechoic and/or hypoechoic aggregation, which may be surrounded by a small anechoic rim.5 Hard tophi can generate well-defined hyperechoic deposits with posterior acoustic shadows, whereas soft tophi can appear hypoechoic with hyperechoic stippled aggregates or bright dotted foci without a posterior acoustic shadow.6
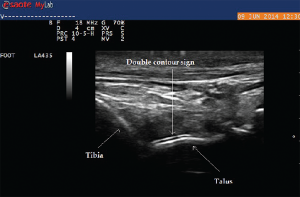
Urate deposition within the synovial tissue can also generate hyperechoic aggregates with a cloudy surrounding rim of hypoechoic signal, with the appearance of wet clumps of sugar. The most specific and helpful finding is the double contour sign, which is a hyperechoic band over the superficial surface of the cartilage reflecting urate deposition on the cartilage surface. It can be differentiated from the interface sign because the double contour sign will have a signal thickness and echogenicity similar to subchondral bone signal, which is unchanged with insonation angle.6 In addition, ultrasound can detect minimal amounts of intra-articular synovial fluid appearing as a compressible anechoic collection and can be used for needle guidance, particularly for joints more challenging to aspirate blindly (i.e., ankle, elbow or the root joints, such as the shoulder or hip).

(click for larger image)
Image 8: Right wrist swelling (left) with focal fusiform swelling over the dorsum of the wrist. To the right, you see the needle entering the tenosynovial fluid (in-plane technique). Bottom: The longitudinal view along the course of extensor pollicis longus taken just proximal to Lister’s tubercle, demonstrating compressible fluid (anechoic or dark area), without tenosynovial hypertrophy. Fluid was aspirated using ultrasound guidance, which demonstrated inflammatory fluid (leukocytes=5545/High Power Field) with calcium pyrophosphate crystals on microscopic exam.
Multiple tiny hyperechoic spots in anechoic synovial fluid are thought to be the earliest ultrasound evidence of crystal deposition.7 In the Study for Updated Gout ClAssification CRiteria (SUGAR), funded by the ACR and EULAR, the double contour sign on ultrasound is one of the 10 key discriminating features that have been identified for further study for new gout classification criteria. Ultrasound findings, along with degree of uricemia, add discriminating value and will significantly contribute to more accurate classification criteria for gout.8 In addition, the presence of peri-articular and intra-articular power Doppler signals, synovial hypertrophy, effusion and soft tissue edema are all indicative of synovitis due to acute crystalline inflammation.