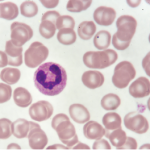
Clonal deletion effectively removes self-reactive B cells from bone marrow. Unfortunately, the system may fail patients with systemic lupus erythematosus (SLE) who develop autoantibodies that form circulating immune complexes with extracellular self-nucleic acids. In some patients, the triggering chromatin is released from dying neutrophils that form neutrophil extracellular traps (NETosis). The expulsion of mitochondrial DNA and associated antimicrobial proteins can serve as autoantigens and drive B cell autoimmune response. Specifically, in patients with rheumatoid arthritis, NET-derived peptides can be citrullinated and may become autoantigenic and recognized by anticitrullinated peptide antibodies.
Clonal deletion effectively removes self-reactive B cells from bone marrow. Unfortunately, the system may fail patients with systemic lupus erythematosus (SLE) who develop autoantibodies that form circulating immune complexes with extracellular self-nucleic acids. In some patients, the triggering chromatin is released from dying neutrophils that form neutrophil extracellular traps (NETosis). The expulsion of mitochondrial DNA and associated antimicrobial proteins can serve as autoantigens and drive B cell autoimmune response. Specifically, in patients with rheumatoid arthritis, NET-derived peptides can be citrullinated and may become autoantigenic and recognized by anticitrullinated peptide antibodies.
In patients with SLE, antibodies to LL37 (anti-LL37) represent one example of circulating anti-neutrophil cytoplasmic antibodies (ANCA) that react to LL37-DNA complexes derived from NETs. The immune complexes deposit into peripheral tissues, where they trigger damaging inflammation and are associated with SLE disease activity.
Although research suggests the neutrophils of SLE patients undergo increased NETosis relative to those from healthy individuals, the relationship between circulating anti-LL37 antibodies and NETosis has not yet been established. Moreover, the mechanism underlying the generation of these antibodies has been unclear until now. New research from Nicolas Gestermann, PhD, a postdoctoral fellow at Lausanne University Hospital, Switzerland, describes a neutrophil-B cell interaction unique to lupus. The description of how NETs directly trigger memory B cells via concerted activation of toll-like receptor 9 (TLR9) and B cell receptor (BCR) to produce anti-NET autoantibody was published in the April issue of The Journal of Immunology.1
“Our study identifies a link between neutrophils, NETs and the activation of self-reactive B cells,” explain the authors in their discussion. “We show that neutrophils undergoing NETosis expose their DNA in complex with the granular antimicrobial peptides. These structures are highly immunogenic and trigger polyclonal B cell activation through TLR9, but also stimulate NET-specific self-reactive B cells by simultaneously engaging the BCR.”
Method
First, the researchers investigated the ability of LL37-DNA complexes present in NETs to trigger the activation of B cells. They found that, although self-DNA alone did not activate B cells, LL37-DNA complexes were able to trigger polyclonal activation of memory B cells. Specifically in individuals with SLE, the LL37-DNA complexes gained access to endosomal compartments of B cells and activated TLR9, thereby triggering polyclonal B cell activation. They also triggered the specific expansion of the self-reactive memory B cell that produce anti-LL37 Abs in an Ag-dependent manner.
Next, the investigators generated NETs by stimulating neutrophils with anti-LL37 Abs. They found the anti-LL37-induced NETs induced strong polyclonal memory B cell activation, as well as the production of IgG antibodies.
The authors propose that patients with SLE have a higher frequency of NET-specific B cells in the B cell memory pool than healthy patients. However, they also note that patients with SLE may have a genetically determined tendency towards increased B cell activation. The study did not determine whether in vivo B cell activation required direct interaction with NETting neutrophils. Nevertheless, the authors suggest NETs or the LL37-DNA complexes may serve as targets for SLE therapy.
Lara C. Pullen, PhD, is a medical writer based in the Chicago area.
Reference
- Gestermann N, Di Domizio J, Lande R, et al. Netting neutrophils activate autoreactive B cells in lupus. J Immunol. 2018 May 15;200(10):3364–3371. Epub 2018 Apr 9.