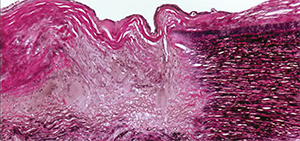
This photomicrograph of the aorta shows transmural destruction on the left side of the specimen with an inflammatory process containing multinucleated giant cells and loss of elastic fibers (Verhoeff-van Gieson stain).
ACR image library
LONDON—New therapies are emerging for the two main forms of large-vessel vasculitis, giant cell arteritis (GCA) and Takayasu’s arteritis—particularly biologic therapies. But for just about every available treatment gap, drawbacks or limited evidence remain, with the results needing to be borne out in larger trials, an expert said at the Annual Congress of the European League Against Rheumatism (EULAR) 2016.
It’s easy to see the need for better options, said Kenneth Warrington, MD, professor of medicine at the Mayo Clinic.
In GCA, glucocorticoids can help with symptoms and inflammatory markers, but those benefits come with vascular complications and even adverse effects, such as increased infection risk and sometimes pneumocystis pneumonia. Plus, relapses are common.1 GCA involves both the TH17 and TH1 pathway, but only one of these is addressed with glucocorticoids.
“Glucocorticoids very effectively abrogate the IL-17 pathway,” he said. “However, they leave the TH1 interferon gamma pathway essentially unchecked and this may lead to chronic smoldering vasculitides that may result in the clinical relapse that we see in our patients. This underscores the importance of more targeted and better therapy for these diseases.”
Similar effects—and problems—are seen with glucocorticoid use in Takayasu’s, he said.
Researchers have found mixed results in trials of methotrexate in GCA, with modest effects in reducing the risk of relapse and a reduction in steroid exposure, Dr. Warrington said.
Data on methotrexate and other conventional immunosuppressive agents in Takayasu’s are particularly thin, coming from a few open-label trials with fewer than 20 subjects per trial, but they show a good initial response followed by frequent relapses and disease progression. Dr. Warrington said that, since patients were also on glucocorticoids, it’s hard to know which therapy was exerting which effects.
Randomized controlled trials have found that TNF inhibitors don’t appear to be effective in GCA.
There is limited evidence that they work in Takayasu’s. One retrospective, multi-center study with 49 patients found a response in 83%, with adverse events in 16%—mostly infections, with two cancer cases.2
And, Dr. Warrington said, “despite the enthusiasm with these drugs, relapses are still seen in about a third.” The field still needs prospective trials on this, he said.
In both GCA and Takayasu’s, responses on IL-6-inhibitors have been seen in about 80% of patients, but with adverse events, including neutropenia and infection, seen in one out of four or five patients, Dr. Warrington said. Use of these therapies also appears to lower glucocorticoid use. And once treatment is ended, relapse is common, he said.
The use of IL-6 inhibitors comes with a special concern in Takayasu’s patients, he warned. Some patients progress even though the symptoms have resolved and inflammatory markers are normal. In one study, three out of 10 relapsed clinically and on radiographic imaging, even though their acute phase markers were normal.3
“Treatment may improve symptoms and markers, but you have to be cautious and follow these patients very closely by clinical evaluation and radiographic imaging studies to monitor for disease progression,” he said.
And again, the field is still waiting for extensive prospective clinical trial data, particularly from the GiACTA trial, which the drug manufacturer sponsoring the study says is the largest trial ever conducted in GCA. The drug manufacturer has issued a statement that the primary endpoint of one-year remission has been met, but detailed information hasn’t yet been shared.
A group in Switzerland recently reported the results from the first randomized, placebo-controlled clinical of tocilizumab in GCA—including 20 patients on active drug and 10 getting placebo. The proportion of patients in remission was significantly greater at 12 and 52 weeks in the active group compared to placebo.4
“This is exciting new data, and we await to see larger data sets,” Dr. Warrington said.
Questions Remain
“A number of unanswered questions remain,” he said. “What is the optimal duration of tocilizumab therapy? What is the effect of tocilizumab on large vessel disease in GCA? What is the response using imaging? And will it prevent vascular complications such as stenosis or aneurysms? I think these are still open for discussion.”
Limited early data show that abatacept, rituximab and ustekinumab show promise in GCA, as well.5 Ustekinumab works by blocking both IL-12 and IL-23—which, Dr. Warrington said, “may be attractive because we’re attacking both the TH17 and the TH1 pathway in large vessel vasculitis.”
In a small trial in refractory GCA patients on ustekinumab, inflammatory markers were not improved, but it allowed patients to greatly reduce glucocorticoid use and come off immunosuppressants.
Even with all these research fronts, there’s still a long way to go in helping patients, Dr. Warrington said.
“There’s a great unmet need in the treatment of large vessel vasculitis,” he said.
“We are enthusiastic and excited about the role of biologics for the treatment of these diseases. But of course we need better biomarkers. We need targeted effective therapy and less toxicity.”
Diagnostic Challenges
Marco Cimmino, MD, associate professor of rheumatology at the University of Genova in Italy, reviewed diagnostic and classification challenges in large vessel vasculitis, emphasizing the amount of overlap seen among GCA, polymyalgia rheumatica, Takayasu’s, isolated ascending aortitis, chronic periaortitis, and IgG4-related disease.
“There are many similarities between these conditions, and one could think that they belong not only to the same family but possibly to the same syndrome,” he said.
A recent study attempted to pinpoint differences between large-vessel GCA (LV-GCA) and classic GCA (C-GCA). Researchers found that those with LV-GCA tended to be younger, with a longer period of symptoms before being diagnosed and more commonly had a history of polymyalgia rheumatica, but a smaller number of them had cranial symptoms. Patients with LV-GCA had a lower rate of blindness but a higher relapse rate and greater steroid doses, researchers found.6
New large-vessel vasculitis biomarkers, which could help with identification and management of the disease, have emerged over the past few years, including pentraxin-3, which has shown high specificity compared to controls and has even shown some ability to differentiate between active disease and disease in remission.7
Promising data have also been generated on antiferritin antibodies and antibodies to the 14-3-3 aorta protein, the newest biomarker candidate, which has been seen frequently in patients with different types of LVV and not often seen in controls, Dr. Cimmino said.8,9
But these biomarkers, he said, “should be studied in the long term to evaluate their prognostic [value].”
Thomas R. Collins is a freelance medical writer based in Florida.
References
- Durand M, Thomas SL. Incidence of infections in patients with giant cell arteritis: A cohort study. Arthritis Care Res (Hoboken). 2012 Apr;64(4):581–588.
- Mekinian A, Comarmond C, Resche-Rigon M, et al. Efficacy of biological-targeted treatments in Takayasu arteritis: Multicenter, retrospective study of 49 patients. Circulation. 2015 Nov 3;132(18):1693–700.
- Goel R, Danda D, Kumar S, et al. Rapid control of disease activity by tocilizumab in 10 ‘difficult-to-treat’ cases of Takayasu arteritis. Int J Rheum Dis. 2013 Dec;16(6):754–761.
- Villiger PM, Adler S, Kuchen S, et al. Tocilizumab for induction and maintenance of remission in giant cell arteritis: A phase 2, randomised, double-blind, placebo-controlled trial. Lancet. 2016 May 7;387(10031):1921–1927.
- Langford C, Cuthbertson D, Ytterberg S, et al. A Randomized Double-Blind Trial of Abatacept and Glucocorticoids for the Treatment of Giant Cell Arteritis. Abstract 9L. Presented Nov. 10, 2015. American College of Rheumatology Annual Meeting. San Francisco.
- Muratore F, Kermani TA, Crowson CS, et al. Large-vessel giant cell arteritis: A cohort study. Rheumatology (Oxford). 2015 Mar;54(3):463–470.
- Ishihara T, Haraguchi G, Kamiishi T, et al. Sensitive assessment of activity of Takayasu’s arteritis by pentraxin3, a new biomarker. J Am Coll Cardiol. 2011 Apr 19;57(16):1712–1713.
- Baerlecken NT, Linnemann A, Gross WL, et al. Association of ferritin autoantibodies with giant cell arteritis/polymyalgia rheumatica. Ann Rheum Dis. 2012 Jun;71(6):943–947.
- Chakravarti R, Gupta K, Swain M, et al. 14-3-3 in thoracic aortic aneurysms: Identification of a novel autoantigen in large vessel vasculitis. Arthritis Rheumatol. 2015 Jul;67(7):1913–1921.

