Myositis Management
One proposed test to help manage myositis patients over time is the IMACS-IIM Disease Activity Core Set, which includes the patient’s and physician’s global assessment of disease activity on a visual analog scale (VAS), MMT8, physical function testing using the Health Assessment Questionnaire (HAQ), laboratory tests for serum activity of muscle enzymes, and assessment for the degree of extraskeletal muscle disease activity using the Myositis Disease Activity Assessment score, Dr. Lundberg said.8
“The 2017 EULAR/ACR classification criteria for myositis were a step forward to harmonize clinical research and clinical trials, but external validation is still needed. One way is to include the new autoantibodies,” she said. “For diagnosis, you still need to use your clinical evaluation, autoantibodies, MRI and muscle biopsy, and all are helpful depending on the different subtypes of myositis and different organ manifestations. As these patients often have multi-organ involvement, they should be managed with a multidisciplinary team, including a physical therapist, rheumatologist, dermatologist [and] pulmonologist.”
Overlapping Myositis
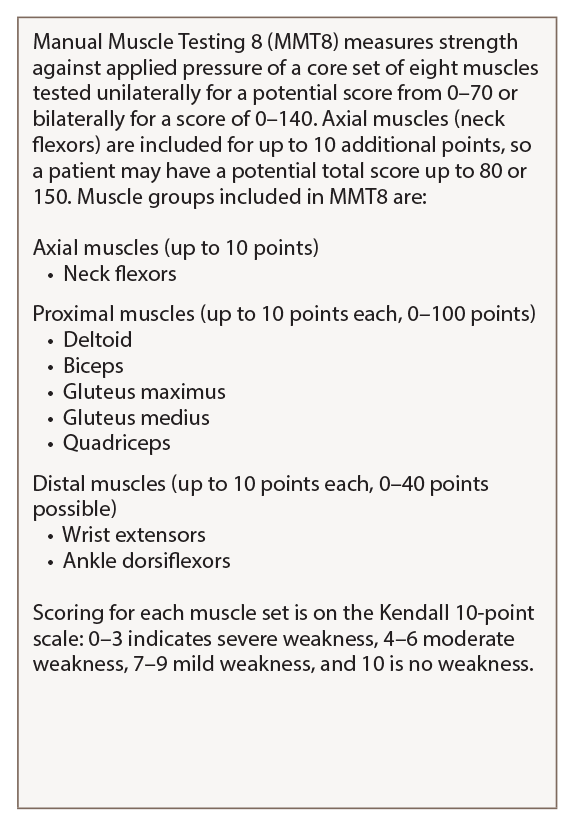
Table 1: MMT8
For a detailed guide on how to perform and score the MMT8, see Manual Muscle Testing Procedures for MMT8 Testing from the National Institute of Environmental Health Sciences.
Myositis may overlap with other rheumatic diseases, most often systemic sclerosis (SSc), but also rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), said Julie J. Paik, MD, MHS, assistant professor of medicine, Johns Hopkins Scleroderma Center and Johns Hopkins Myositis Center.
Researchers have attempted to describe and classify patients with overlap myositis (OM) conditions. A 2005 study found that up to 29% of subjects in a Canadian myositis cohort had an overlap syndrome.9 A 2014 study found that 23% of myositis patients in a Brazilian cohort had overlapping RA and 29% had overlapping SLE, she said.10 “This may include myositis with a few overlapping connective tissue disease features, such as Raynaud’s phenomenon, arthritis, ILD, and a few features of SSc and lupus,” or on the other hand, patients met strict criteria for both myositis and the overlapping condition such as scleroderma, she said.
Rheumatologists first published research on cases of OM in scleroderma 50 years ago.11,12 The prevalence of muscle weakness in these patients broadly varies—from 5% to 95%—in studies due to the lack of consensus classification criteria for overlap myositis, said Dr. Paik.
“Another reason for the broad range of the prevalence is that the patients have previously been assessed solely by having abnormal muscle enzymes alone or an abnormal EMG, MRI or muscle biopsy,” she said. “While previously underappreciated in scleroderma, it is now increasingly recognized that myopathy is a poor prognostic feature in systemic sclerosis.” In a large Canadian scleroderma cohort, mean survival time was much shorter in patients with an elevated CK of ≥200 or physician-reported history of myopathy. Other clinical features that impacted survival in this study were early diffuse SSc, topoisomerase 1 positivity, ribonucleoprotein positivity, ILD and male gender.13
To learn more about OM in SSc patients’ long-term outcomes, Dr. Paik and her colleagues at Johns Hopkins Scleroderma Center recently conducted a nested, case-control cohort of 1,718 scleroderma patients from 1990 to 2012, and identified 392 that had muscle weakness, as defined by a Medsger Muscle Severity Score of ≥1 (which indicates at least 4/5 strength on the MRC scale). The primary outcome of interest was the HAQ-DI, a validated patient reported outcome of disability.14
“The classic phenotype of these patients who had muscle weakness was that they were African American, have shorter disease duration and diffuse subtype. Weak patients also tended to have a higher burden of disease, with severe GI [gastrointestinal] involvement, a history of renal crisis, synovitis, more restrictive lung disease, higher RVSP [right ventricular systolic pressure], an ejection fraction of less than 50% and higher CK elevations. Not surprisingly, weak patients tended to have a higher HAQ-DI score,” said Dr. Paik.
The researchers also looked at these patients’ autoantibodies and found that anti-centromere positivity was somewhat protective. While both weak and non-weak patients had similar levels of most scleroderma-specific autoantibodies, weak patients tended to have a high anti-nuclear antibody (ANA) titer with a nucleolar pattern, she said.
As patients’ muscle severity scores rose, the researchers saw a matching rise in HAQ-DI scores. This connection was seen even when they controlled for confounders like age, gender, restrictive lung disease and synovitis.
In a subsequent study, they wanted to explore the etiology of muscle weakness in the 42 of 65 SSc patients who had had a muscle biopsy read at Johns Hopkins Scleroderma Center.15 In addition to analyzing the muscle biopsy characteristics of these patients, the electrophysiologic characteristics of these patients were also studied. On EMG about 48% of these patients had an irritable myopathy, and “surprisingly, we found that on nerve conduction results, 43.5% had an abnormal sural amplitude, meaning that they had no response when the sural nerve was stimulated, or if the sural amplitude was less than 5,” said Dr. Paik. In patients with a myopathy, researchers typically expect such “myopathic findings” on EMG only, not neuropathy. Both EMG and nerve conduction studies are performed on weak patients to determine the etiology of the weakness. When they reviewed these patients’ EMG data, they only expected to see signs of a muscle problem, not a nerve problem.
“When we looked at the individual muscle biopsy features, we found that necrosis was predominant, at 66%,” followed by inflammation, she said. Nearly half the weak patients also had acute neurogenic atrophy, which suggests that motor denervation may be a common pathologic process in weak SSc patients. “We then combined the aggregate individual histologic features and found that the most common histopathologic category was non-specific myositis (35.7%) and necrotizing myopathy (21.4%),” she said. Three patients had fibrosis only, which led the researchers to explore this unique histologic subset of scleroderma.

