Fibrosing Myopathy
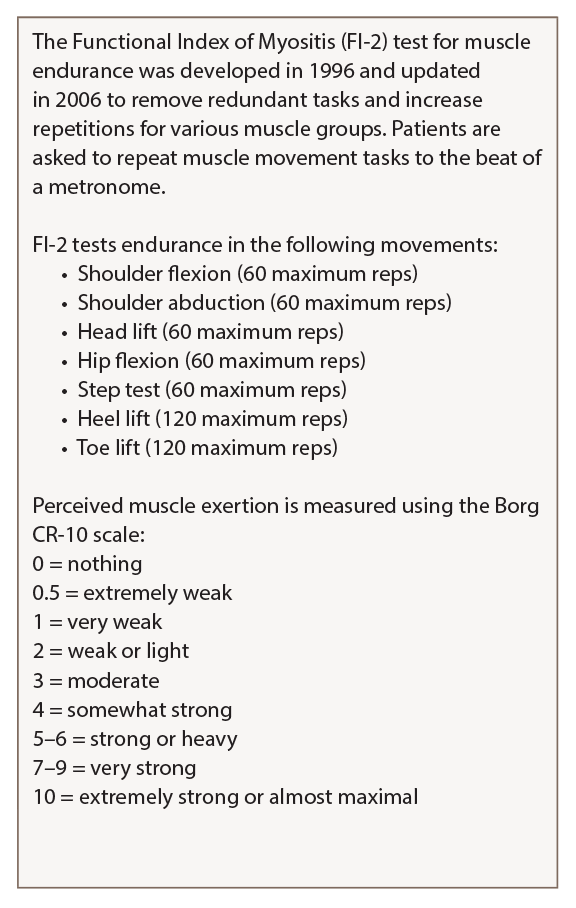
Table 2: Functional Index of Myositis
Karolinska Institute in Stockholm created a detailed guide on how to perform and score the FI-2 test that is available on the National Institute of Environmental Health Science website.
“After we found those three cases, we started to do a more systematic assessment of muscle weakness in all our scleroderma patients, and we started to see that, when we did biopsies, we started to see more of these patients,” said Dr. Paik. “So, we coined the term fibrosing myopathy, where we see fibrosis only and a lack of inflammatory infiltrates.” These patients’ fibrosis is primarily perimysial and endomysial, and thick, dense connective tissue encases the muscle fascicle, she explained.
In a 2017 study designed to further understand the clinical phenotype of fibrosing myopathy, the researchers compared these patients with those with an inflammatory myopathy, defined as inflammation and/or necrosis.16
“We saw that the fibrosing myopathy patients tended to be of the diffuse subtype, African American, and their duration of follow-up was really short—1.86 years vs. 5.93 years after a muscle biopsy, because most of them, unfortunately, were deceased.” They determined that fibrosing myopathy was associated with higher mortality. These patients also had elevated troponin, as well as lower CK and aldolase than those with inflammatory myopathy. They also identified two autoantibodies seen in fibrosing myopathy patients: anti-Scl-70 and anti-U3-RNP. The five deceased patients in the study all died of non-ischemic cardiomyopathy. Of the three patients who are still living, two are being treated with mycophenolate mofetil and intravenous immunoglobulin (IVIG), and doing well, and one is doing well on MMF alone, said Dr. Paik.
Another 2017 study determined that fibrosis was the predominant feature on muscle histopathology in 35 SSc patients, with 81% of SSc patients having fibrosis compared to 32% of patients with inflammatory myopathy.17
“Similar to our study, perimysial and endomysial fibrosis were the predominant finding,” said Dr. Paik. “They took it to another level, testing for TGF-β and type-I collagen, and they were also more prevalent in the patients who had scleroderma. In addition, because of the intense vasculopathy seen in patients with scleroderma, they also looked at VEG-F [vascular endothelial growth factor], and it was also increased in those patients with significant fibrosis.” Electron microscopy showed that these patients’ endothelial cell swelling exhibited microangiopathy and thickened basement membrane, as well as intense fibrosis in the endomysium and perimysium.
Patients with fibrosing myopathy have lower muscle enzymes, which may make it difficult for rheumatologists to diagnose this form of myopathy early, Dr. Paik said. While the optimal treatment algorithm for OM in SSc is unknown, “one thing is certain: We should not give high-dose steroids to our patients with scleroderma, because of the high risk of renal crisis. So we need to choose a steroid-sparing agent that can treat the skin and muscle,” she said.

