The extent and experience of pain is influenced by affective, behavioral, and cognitive processes. Thus, there are numerous factors to consider in pain management; however, the role of sleep may be one of the most important. There is good evidence that sleep, pain, and depression form a tightly interconnected triad where changes in one of the three can impact the other two. For example, disturbed sleep can result in increased pain and contribute to changes in mood, while persistent pain can contribute to poor sleep and a depressed mood.
Sleep disturbances are common even in healthy individuals. The prevalence of insomnia in the U.S. population has been estimated to be higher than 10%, but people with chronic illnesses are at an even greater risk. A recent study reported that 23% of adults with arthritis experience insomnia.1 This same study found that those with arthritis and depression or anxiety were at the highest risk for disturbed sleep. As might be expected, joint pain and limitations due to pain mediated the relationship between arthritis and sleep.1 Conversely, sleep disruption can reduce pain threshold and contribute to other symptoms like fatigue, cognitive fogginess, and irritability, as well as diminished functioning and overall decreased quality of life.2

Evaluating sleep in rheumatologic patients can begin with a single self-report item on intake or follow-up forms. We use the “waking up tired (unrefreshed)” item from the Symptom Severity scale that is part of the survey criteria for fibromyalgia.3 Responses suggesting disturbed sleep can be further explored by assessing the number of hours of sleep per night, ability to fall asleep, and waking patterns throughout the night. Further, some patients have other specific conditions that account for sleep disturbances, such as sleep apnea or restless legs syndrome, which should be evaluated and addressed when present. Validated measures such as the Pittsburgh Sleep Quality Index or the Medical Outcomes Study Sleep Scale can be used in clinical practice for both initial evaluation and assessment of improvement posttreatment.4
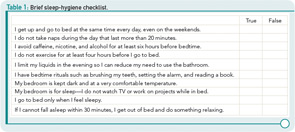
After considering the nature of the sleep disturbance, behavioral interventions may prove to be a low-cost and effective solution. To determine what behavioral changes might be needed, an assessment of general “sleep hygiene” can be conducted. Sleep hygiene refers to the practice of maintaining good habits that are conducive to sleep. Often, patients with chronic pain develop bad habits with regard to their sleep, such as taking long naps during the day, drinking too much caffeine to combat fatigue, or engaging in stressful activities too close to bedtime. Table 1 shows a list of behaviors generally considered essential for good sleep hygiene. These behaviors appear in a checklist format that can be adapted for use in the clinical setting.
Once you’ve identified the problem behaviors, encourage your patient to make changes and set concrete, but easily achievable, goals. It can be helpful to reassure patients that millions of people experience sleep disturbances and that the good news is that sleep problems can be frequently addressed with behavioral changes alone. If patients do not respond to simple sleep hygiene interventions, a referral to cognitive-behavioral therapy could be a good next step.
Dr. Hassett is an associate research scientist in the department of anesthesiology at the University of Michigan Medical School and Chronic Pain and Fatigue Research Center in Ann Arbor, Mich.
References
- Louie GH, Tektonidou MG, Caban-Martinez AJ, Ward MM. Sleep disturbances in adults with arthritis: Prevalence, mediators, and subgroups at greatest risk. Data from the 2007 National Health Interview Survey. Arthritis Care Res. 2011;63:247-260.
- Chiu YH, Silman AJ, Macfarlane GJ, et al. Poor sleep and depression are independently associated with a reduced pain threshold. Results of a population based study. Pain. 2005;115:316-321.
- Wolfe F, Clauw DJ, Fitzcharles MA, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: A modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38:1113-1122.
- Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med. 2005;6:41-44.