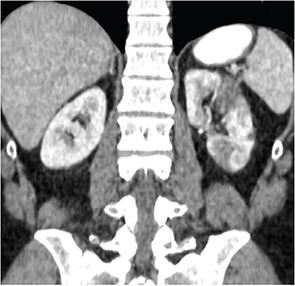
On examination, he was afebrile, and his blood pressure was 145/85 mmHg with a heart rate of 121 beats per minute. He had easily visible veins on his shoulders, chest and abdomen but no hyperextensible joints. The remainder of the examination was unremarkable. Repeat laboratory testing revealed a thrombocytosis to 410 (ref. 150–400th/cu mm), ESR of 7 mm/hr (ref. <13 mm/hr) and a CRP of 35.2 mg/L (ref. <6 mg/L).
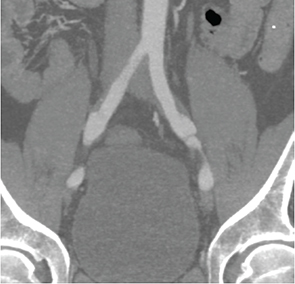
Note bilateral dissections of the common iliac arteries with surrounding soft tissue thickening.
Differential Diagnosis
We were faced with a patient who presented with multifocal dissections with associated inflammatory vessel wall changes as well as elevated inflammatory markers. Treatment with prednisone led to a decrease (although not complete resolution) of inflammatory marker elevations and resolution of some inflammatory changes; however, there was progression of the left common iliac artery dissection. A number of possible etiologies were considered, which can be broadly divided into vasculitides and noninflammatory vasculopathies.
Vasculitis
The most common vasculitis affecting the large vessels in an individual younger than 50 years is Takayasu arteritis (TAK). However, a number of other vasculitides, including Behçet’s and polyarteritis nodosa, can affect the large vessels, such as the renal and iliac arteries. Our patient did not have oral ulcerations to suggest Behçet’s or other signs or symptoms to suggest polyarteritis nodosa. Despite the elevated inflammatory markers, we felt that TAK was less likely because the inflammatory changes on imaging were limited to the areas of dissection and spared other vascular beds affected by TAK, particularly the aorta, subclavian and axillary arteries.1 Although TAK can lead to dissections, the most common arterial lesions are stenoses, which were not seen in our patient. In addition, 80–90% of patients with TAK are women, further decreasing the likelihood of this condition.1
Because our patient’s presentation was not consistent with a primary vasculitis, we felt that the elevated inflammatory markers and inflammatory changes surrounding the vessels on imaging were most likely secondary to the dissections, rather than primary manifestations of the underlying illness. These considerations raised our concern for a noninflammatory vasculopathy as the unifying diagnosis.
Noninflammatory Vasculopathies
Noninflammatory vasculopathies affecting the large vessels are a heterogeneous group of disorders and include Ehler’s Danlos Type IV (EDS IV), Marfan’s syndrome, Loeys-Dietz syndrome, fibromuscular dysplasia (FMD) and segmental arterial mediolysis (SAM). In addition, atherosclerotic lesions can lead to aneurysm and dissection and must be considered in the differential.