Two common leisure activities that people do in sitting for more than 30 minutes include screen-time activities (e.g., watching TV/movies, playing video games, surfing the Web on their computer or mobile device) and reading.
Standing up & stretching during TV commercials & after each computer game or chapter in a book & limiting leisure screen-time activities to less than two hours a day are simple ways to reduce leisure-time sedentary behaviors.
Three common occupational activities that people do while sitting for more than 30 minutes include working at a desk/computer, meetings and commuting for work. It’s easy to reduce occupational sitting by standing up and stretching every half hour when working at the computer and during meetings, standing up to talk on the phone, using the stairs (e.g., one floor up, two floors down), and having standing or walking meetings.
- Adding 100 steps or 50 meters of slow leisurely walking to home and work activities will reduce sedentary time by two minutes. Try walking 50 meters (i.e., the length of an Olympic-sized swimming pool or a short city block) to and from five home- or work-based activities. This will add 1,000 steps or 20 minutes of light activity into your day.
You Won’t Know If You Don’t Ask: 2 Simple Screening Questions
Physical Activity Screening Question: In the past week, approximately how many days did you do at least one walking or other moderate-to-vigorous physical activity that lasted 10 minutes or more? Note: In other words, your heart rate, breathing and body temperature would have increased slightly during the activity, but you could still talk without difficulty while doing the activity.
Interpretation
- Active: five to seven days with 20–30-plus minutes of moderate-effort activity.
- Fairly Active: five to seven days a week with 10–20 minutes of moderate-effort activity.
- Less Active: three to four days a week with 10–20 minutes with moderate-effort activity.
- Inactive: two or fewer days a week with 10–20 minutes of moderate-effort activity.
Sedentary Behavior Screening Question: In the past week during your leisure time, approximately how many hours a day did you spend sitting or lying still doing screen-time-related activities? Note: Screen-time activities include watching TV/movies, playing video games or surfing the Web on your computer or mobile device.19
Routinely asking patients about their normal physical activity & sedentary behaviors will help you understand when & what additional information or support may be needed to assist them to become more active & sit less throughout the day.
Interpretation
- Very Sedentary: >two hours a day of leisure screen-time activities.
- Sedentary: one to two hours a day of leisure screen-time activities.
- Minimally Sedentary: less than an hour a day of leisure screen-time activities.
- Non-Sedentary: no leisure screen-time activities.

What You Can Do
You can help people living with RA develop and maintain a physically active lifestyle. Some tips:
- Active: Acknowledge that the person is likely meeting PA guidelines and encourage ongoing physical activity. Ask about how much higher-intensity/vigorous activity they are doing each week, and refer them for advice if they are possibly doing too much exercise (i.e., complaining of joint pain or increased fatigue after vigorous activities).
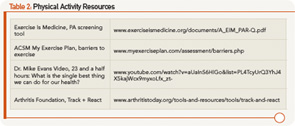
- Fairly Active: Acknowledge that the person is close to meeting PA guidelines, and encourage an ongoing physically active lifestyle. Offer some individualized advice and support for ways to increase their PA, and provide information and resources that will help them maintain their motivation (see Table 2).
- Less Active: Explore the person’s readiness and motivation to change their PA behaviors, and explore their possible barriers to being more physically active (see Table 2). Provide some individualized support with problem solving, goal setting and action planning to improve their PA behaviors or refer them to an arthritis-trained health professional to provide this support.
- Inactive: Refer them to an arthritis-trained health professional to assess the person’s readiness and motivation to change their PA behaviors and explore possible barriers to being more physically active through individualized support to increase their activity.
Some tips for how you can support people living with RA to be less sedentary:
- Non-Sedentary: Ask about other sitting behaviors/activities besides screen-time activities that they may be doing for long periods of time during their leisure time. Acknowledge their non-sedentary lifestyle, and reiterate the important health benefits of doing a little bit of activity frequently throughout the day. Encourage pacing, rest and energy conservation as important elements of self-management in RA.
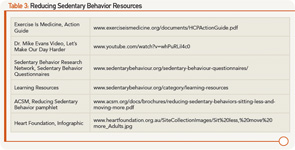
- Minimally Sedentary: Ask about other sitting behaviors/activities as above and acknowledge their minimally sedentary lifestyle. Discuss the health benefits of doing a little bit of activity frequently throughout the day. Provide additional information on and resources for ways to reduce sitting in their day (see Table 3).
- Sedentary: Explore the person’s readiness and motivation to change their sedentary behaviors and discuss possible reasons for or barriers to not reducing their sedentary behaviors (see Table 3). Provide some guidance or support on reducing sedentary time or refer them to an arthritis-trained health professional who can provide more individualized support through problem solving, goal setting and action planning.
- Very Sedentary: Refer them to an arthritis-trained health professional for an evaluation of readiness and motivation to change their sedentary behaviors and overcome their barriers to reducing sedentary behaviors, and individualized support to reduce sedentary behavior.
Summary
Encouraging more physical activity and less sitting throughout the day are equally important health and lifestyle messages that we should reinforce with every patient living with RA. To support our RA patients to exercise more and sit less, it’s important that we understand what these messages mean in terms of actual behaviors to screen for and encourage in our patients. It is particularly important to refer newly diagnosed RA patients or those with moderate to higher levels of disease activity to an arthritis-trained health professional for individualized support and guidance on safe and appropriate physical activities and minimizing sedentary behaviors.