Rheumatologists and many other physicians are deeply concerned about the decrease in Medicare reimbursement for dual energy X-ray absorptiometry (DXA) and vertebral fracture assessment (VFA) that took effect on January 1. The current reimbursement schedule will reduce practice expense reimbursement from the 2006 levels of approximately $140 for DXA and $40 for VFA to $40 and $25, respectively, by 2010—less than it costs to actually perform and interpret the tests.
“The proposed rates of reimbursement simply will not make up the expense of doing it in the physician’s office,” says Steven Petak, MD, president of the American Academy of Clinical Endocrinologists (AACE), and immediate past president of the International Society for Clinical Densitometry (ISCD). “If this goes into effect, my practice may have to stop seeing new Medicare patients. It’s a heartbreaking decision, but otherwise we’d go bankrupt.”
The cuts are due in part to a program of general governmental belt tightening mandated by bill S.1932, better known as the Deficit Reduction Act of 2005 (DRA). The DRA resulted from a congressional budget resolution to reduce spending by about $35 billion from 2006 to 2010. According to Congressional Budget Office estimates, enacting the DRA as written would reduce direct congressional spending by a total of $99 billion from 2006 through 2015. The net savings on Medicare and Medicaid combined over that time period would be $11.2 billion.
The bill requires reimbursement for imaging services to be cut by a total of $2.8 billion from 2007 to 2010, and by $8.1 billion through 2015. This would be accomplished, in part, by capping payment for the technical component of the exam—that is, the actual performance of the examination, rather than the interpretative aspect—at the rates paid for an exam performed in a hospital, even if it is actually performed in a physician’s office. Congress lumped DXA and VFA in with other imaging studies like PET and CT, even though the bone-density exams are simpler and less expensive to perform.
Additional reimbursement cuts to DXA happened through the Centers for Medicare & Medicaid’s (CMS’) five-year review process and when CMS changed the way it calculates practice expense.
Why a Reduction?
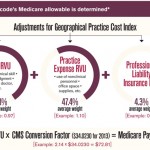
Every five years, the CMS must review the rates at which Medicare reimburses doctors for various treatments and procedures and, when necessary, adjusts them to reflect changes in technology, utilization, and other factors. The Medicare Physician Fee Schedule has three components: work, consisting of the actual physician work of performing a given treatment or test; practice, such as non-physician work time, equipment and supplies; and professional liability. In 2006, CMS also had to take into account the provisions of the DRA as it determined what changes, if any, to make in the work and practice portion of the fee schedule. To help guide their decisions, CMS officials rely on advice from the Relative Value Scale Update Committee (RUC) convened by the AMA. The RUC, in turn, makes recommendations based on its examination of any new data and the opinions of expert consultants.