sciencepics/shutterstock.com
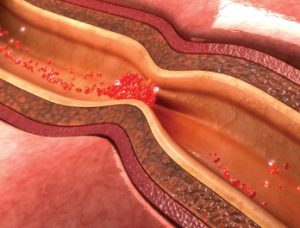
Complement can deposit in various tissues, and previous studies have associated complement deposition with an increased risk for all-cause mortality and stroke. Now, new research underscores the relationship between rheumatic disease, the complement system and cardiovascular disease. In particular, inflammatory rheumatic disease status appears to be uniquely associated with mononuclear cell infiltrates in the vascular system, as well as observable C3d deposition.
Kelly J. Shields, PhD, of the Allegheny Health Network in Pittsburgh, and colleagues published the results of their analysis of complement in patients with rheumatic disease and coronary artery disease online March 31 in Plos ONE.1 Their cross-sectional study included 60 patients with systemic lupus erythematosus (SLE) and/or rheumatoid arthritis (RA).
“To our knowledge, this is the first study to evaluate complement protein deposition within the vessels of SLE, RA and non-[inflammatory rheumatic disease] patients with [coronary artery disease],” write the authors in their discussion. “The findings support the unique relation between complement and [inflammatory rheumatic disease], in particular SLE. From these findings, two important questions arise, which include the source and the targets of the complement and the complement activation products.”
The investigators sorted patients into one of three groups: those with inflammatory rheumatic disease but without coronary artery disease, those with coronary artery disease but without inflammatory rheumatic disease, and those with both inflammatory rheumatic disease and coronary artery disease. The median age of patients was 57 years in the group with inflammatory rheumatic disease but without coronary artery disease, 70 years in the group with coronary artery disease but no inflammatory rheumatic disease and 70.5 years in the group with both. The researchers noted that patients with SLE and/or RA who also had coronary artery disease experienced a higher number of myocardial infarctions than those in the group with coronary artery disease but without inflammatory rheumatic disease.
Patients in the group with both diseases also had higher circulating levels of systemic inflammatory biomarkers than patients in the other two groups. Moreover, their circulating C3 was associated with inflammatory rheumatic disease duration. In the case of patients in the group with coronary artery disease but without inflammatory rheumatic disease, circulating C3 levels were positively associated with body mass index and C-reactive protein. The researchers also reported that inflammatory rheumatic disease was significantly related to the presence and size of mononuclear cell infiltrates, such that inflammatory rheumatic disease was strongly associated with the presence of mononuclear cell infiltrates ≥50 in the aortic adventitia. Moreover, the presence of mononuclear cell infiltrates was related to C reactive protein and the presence of ≥50 mononuclear cell infiltrates was associated with hypertension and current smoking.
