Many patients present to the office with foot complaints not related to any rheumatological condition. It’s common to categorize foot problems in three anatomic areas: forefoot (i.e., from the metatarsal bases to the toes), midfoot (i.e., cuneiforms, cuboid and navicular) and hindfoot or rearfoot (i.e., talus and calcaneus). Common forefoot conditions include hallux valgus, hallux rigidus, interdigital neuroma (i.e., Morton’s neuroma) and metatarsalgia. Plantar fasciitis, inferior and posterior calcaneal bursitis, and Achilles tendonitis affect the rearfoot. This article focuses on the management of some of these common issues.
The management of all of these conditions is similar, and treatment recommendations for all of them include rest, nonsteroidal antiinflammatory drugs (NSAIDs), stretching, over-the-counter inserts, physical therapy, heel lifts, custom orthotics and/or accommodative orthotics. The two most critical recommendations are the use of properly fitted/supportive footwear and weight loss.
The most common cause of foot pain is ill-fitting, nonsupportive shoes. When questioned, most patients cannot recall when they last had their feet professionally sized at a shoe store. Recommending to your patients that they wear an appropriately fitted shoe for a specific activity will likely do more to help the patients’ foot complaints than anything else you recommend or prescribe—if the patient complies.
The clinical presentation of hallux rigidus includes a limited range of motion with pain in the first metatarsal phalangeal joint.
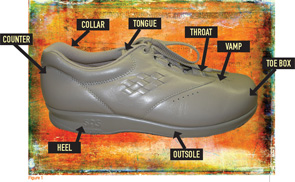
I recommend checking shoe size (i.e., length and width), choosing the proper shoe for the intended activity, obtaining a shoe stretcher for any deformity (e.g., bunion or hammertoe), using accommodative devices (e.g., silicon pads) for deformities and wearing accommodative shoes with extra depth in the toe box for forefoot deformities. The shoe should have a firm, supportive heel counter and not be too flexible in the sagittal and frontal planes. A wide Blucher opening allows room for swelling and is easier for the patient to take on and off (see Figure 1, above).
Referral to a registered dietician for nutrition counseling and implementation of a subsequent weight loss program are also essential to reduce stress on the foot. Treatment strategies for some common issues are presented below.
Hallux Rigidus
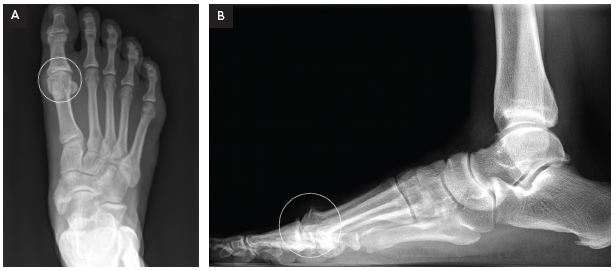
The clinical presentation of hallux rigidus (see Figures 2A and 2B, p. 32) includes a limited range of motion with pain in the first metatarsal phalangeal joint (MTP). The pain is usually felt in and around the joint. Frequently, a noticeable enlargement of the first MTP occurs. The patient will complain of an inability to wear shoes and difficulty wearing heels or boots. Radiographs will demonstrate osteoarthritic changes in the joint.