Many patients present to the office with foot complaints not related to any rheumatological condition. It’s common to categorize foot problems in three anatomic areas: forefoot (i.e., from the metatarsal bases to the toes), midfoot (i.e., cuneiforms, cuboid and navicular) and hindfoot or rearfoot (i.e., talus and calcaneus). Common forefoot conditions include hallux valgus, hallux rigidus, interdigital neuroma (i.e., Morton’s neuroma) and metatarsalgia. Plantar fasciitis, inferior and posterior calcaneal bursitis, and Achilles tendonitis affect the rearfoot. This article focuses on the management of some of these common issues.
The management of all of these conditions is similar, and treatment recommendations for all of them include rest, nonsteroidal antiinflammatory drugs (NSAIDs), stretching, over-the-counter inserts, physical therapy, heel lifts, custom orthotics and/or accommodative orthotics. The two most critical recommendations are the use of properly fitted/supportive footwear and weight loss.
The most common cause of foot pain is ill-fitting, nonsupportive shoes. When questioned, most patients cannot recall when they last had their feet professionally sized at a shoe store. Recommending to your patients that they wear an appropriately fitted shoe for a specific activity will likely do more to help the patients’ foot complaints than anything else you recommend or prescribe—if the patient complies.
The clinical presentation of hallux rigidus includes a limited range of motion with pain in the first metatarsal phalangeal joint.
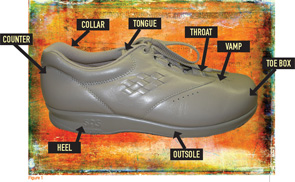
I recommend checking shoe size (i.e., length and width), choosing the proper shoe for the intended activity, obtaining a shoe stretcher for any deformity (e.g., bunion or hammertoe), using accommodative devices (e.g., silicon pads) for deformities and wearing accommodative shoes with extra depth in the toe box for forefoot deformities. The shoe should have a firm, supportive heel counter and not be too flexible in the sagittal and frontal planes. A wide Blucher opening allows room for swelling and is easier for the patient to take on and off (see Figure 1, above).
Referral to a registered dietician for nutrition counseling and implementation of a subsequent weight loss program are also essential to reduce stress on the foot. Treatment strategies for some common issues are presented below.
Hallux Rigidus
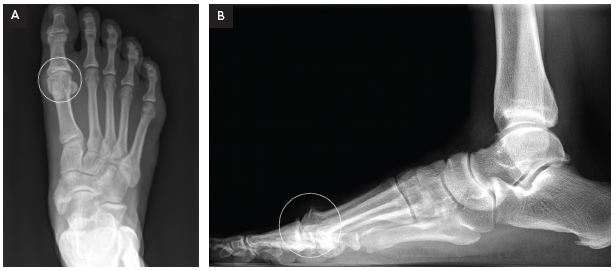
The clinical presentation of hallux rigidus (see Figures 2A and 2B, p. 32) includes a limited range of motion with pain in the first metatarsal phalangeal joint (MTP). The pain is usually felt in and around the joint. Frequently, a noticeable enlargement of the first MTP occurs. The patient will complain of an inability to wear shoes and difficulty wearing heels or boots. Radiographs will demonstrate osteoarthritic changes in the joint.
Treatment recommendations include a change in footwear (i.e., extra-depth toe box), shoe stretcher, Achilles runner’s or calf stretch (i.e., gastrocnemius-soleus stretch), heel lifts, NSAIDs and shoe inserts with a Morton’s extension (i.e., an extension under the great toe). If pain persists, an intra-articular steroid injection may be helpful. If conservative treatment fails, refer the patient to a podiatrist for a surgical consultation.

Metatarsalgia
With metatarsalgia, there is generalized forefoot pain involving the lesser metatarsals and MTPs. The lateral squeeze test may also elicit pain. The differential diagnosis includes intermetatarsal bursitis, fractures (e.g., traumatic or stress), osteochondritis of the metatarsal head (e.g., Freiberg’s) (see Figure 3, below), bone neoplasm, interdigital neuroma and vascular insufficiency.
Metatarsal stress fractures (see Figure 4, below right) present with swelling, erythema and pinpoint tenderness on the metatarsal shaft. Initial radiographs may not demonstrate any evidence or indication of a stress fracture. Diagnosis is often based on the clinical presentation and the physician’s judgment. Treatment by immobilization in a post-op shoe or short cast boot for four to six weeks is recommended. Interval radiographs can help determine the progression of healing.
Neuroma
Patients with an interdigital neuroma complain of pain, burning and tingling in and around the third interspace radiating to the third and fourth toes, along with a sense of plantar fullness. Manipulation of the interspace resulting in a palpable click that duplicates the pain is known as a Mulder’s sign. Recommendations for treatment include using proper footwear, a metatarsal pad, NSAIDs and Achilles runner’s stretch. A steroid injection to the interspace may be helpful. If these conservative measures fail, the patient may be referred to a podiatrist for surgery.
Rearfoot Problems
The majority of rearfoot problems (e.g., plantar fasciitis, inferior and posterior calcaneal bursitis and Achilles tendonitis) are mechanical in origin. Trauma, neurological conditions and arthritis are other causes of rearfoot pain. Rest, ice, compression, elevation, proper footwear, physical therapy, night splints, NSAIDs, over-the-counter orthotics, orthopedic heel lifts, heel cushions and Achilles calf stretch can be very effective in the treatment of all of these conditions.
If the patient has a posterior heel spur or bursitis, a two-way shoe stretcher and/or a posterior silicon heel protector may be useful.
The Fundamentals
Rheumatologists often see patients who present with forefoot, midfoot and rearfoot conditions unrelated to any rheumatological condition. Key treatment recommendations for all such conditions include the use of properly fitted/supportive footwear and weight loss, along with rest, NSAIDs, stretchers, inserts, orthotics and physical therapy.
James P. Ioli, DPM, is chief of the Division of Podiatry at Brigham and Women’s Hospital in Boston and assistant professor of orthopedic surgery at Harvard Medical School.
Resources
- Jenkin, WM. Approach to the Patient with Ankle & Foot Pain. In: Imoboden JB, Hellmann DB, Stone JH. eds. Current Rheumatology Diagnosis and Treatment, 2nd ed. McGraw Hill, New York; 2007.
- Klippel JH, Dieppe PA, et al, eds. Rheumatology, 2nd ed. Mosby, St. Louis, Mo.; 1998.
- Southerland JT, Boberg JS, Downey MS, et al. McGlamry’s Comprehensive Textbook of Foot and Ankle Surgery, 4th ed. Kluwer, Lippincott, Williams and Wilkins, Philadelphia; 2012.